Insights in Blood Disorders
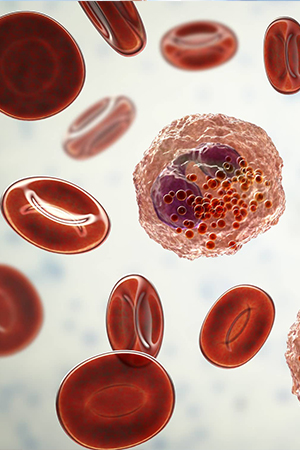
Open AccessCytogenetic and Molecular Features of Mixed Phenotype Acute Leukemia and the Impacts of Targeted Therapy
Authors: Jordan Selep DO, Zoe McKinnell, Seta Degann, Daniel Karel, Shanshan Liu, Guoqing Diao, Martha Antonio, Amarendra Neppalli, Samah Nassereddine, Maneesh Rajiv Jain.
Abstract
Background: Currently, there is no treatment consensus on the optimal treatment regimen for mixed-phenotype acute leukemia (MPAL).
Aims: To analyze the cytogenetic and molecular characteristics of U.S. veterans diagnosed with MPAL as well as examine the effects of targeted therapy on their overall survival.
Methods: Retrospective study between the years 2000-2023
Setting: U.S. Department of Veterans Affairs
Participants: United States veterans in the Veterans Affairs Informatics and Computing Infrastructure (VINCI) database diagnosed with MPAL between 2000-2023. The text utilization integration feature was used to query all notes which included the phrases “mixed phenotype acute leukemia”, “MPAL”, and “biphenotypic leukemia” and identified 320 patients. All patient charts were reviewed manually. 94 patients were included in the final analysis.
Exposure: Treatment for MPAL.
Main outcomes and measures: The primary outcome was 5-year overall survival (OS), KaplanMeier and Cox regression analyses were used to compare this between different patient groups.
Results: Of the 74 patients treated with curative intent, 33 patients had potentially targetable mutations and 21 patients received targeted therapy. The 5-year OS for the entire cohort was 26%. Mutations noted in more than one patient included RUNX1 (n=10), NOTCH1 (n=4), DNMT3A (n=4). For the purposes of the study, TP53, TET2, and inv(16) were removed from the model due to small number of positive patients. Patients with Ph, RUNX1, and FLT3 mutations had improved OS with HR of 0.21 (p=<0.001), 0.43 (p=0.15), and 0.65 (p=0.5) respectively.
Patients older than 60 years in age had poorer outcomes, HR 1.06 (p>0.09) with patients older than 80 years in age, with the worst outcomes, HR 11.9 (p=0.008).
Patients who were sent to transplant in their first clinical remission (CR1) had better outcomes with HR 0.14 (p=<0.001), while patients who required salvage chemotherapy had worse outcomes, as expected, with a HR of 7.59 (p=<0.001).
Conclusions and Relevance: Molecular and cytogenetic testing may be beneficial for use in the treatment of MPAL; sending patients to transplant in addition to using targeted therapy has the most beneficial outcome.
Editor-in-Chief

View full editorial board →