Acute Ischemic Stroke as Complication of Untreated Infant with Cyanotic Congenital Heart Disease, Case Report
Author'(s):Dr. Huda Khaleel MD* and Dr. AlQassmi Amal MD
Dr. Huda Khaleel MD* and Dr. AlQassmi Amal MD
*Correspondence:
Huda Khaleel, Pediatric Cardiology, King Saud Medical city/ Riyadh.
Received:29 November 2019; Accepted:29 November 2019;
Citation: Huda Khaleel, AlQassmi Amal. Acute Ischemic Stroke as Complication of Untreated Infant with Cyanotic Congenital Heart Disease, Case Report. Addict Res. 2019; 3(1): 1-4.
Abstract
Background: Stroke is a common presentation in emergency department but rarely seen in pediatric patients. In case of acute ischemic stroke in pediatric age group, management is different from that of adult ischemic stroke where thrombolysis is a good option.
Method: We report Term baby, 28days old baby had history of fever for 3 days after delivery and lethargy, irritability, poor feeding associated with cyanotic spell, apnea for few seconds after few days of admission had frequent multifocal seizure (tonic-clonic)of both limbs diagnosed to D-TGA complicated with have right partial stroke and deep venous thrombosis.
Result: Patient improved clinically and refer to tertiary center for cardiac surgery.
Conclusion: Cyanoticheart lesions not only increase the risk of cerebral infarction, but can also mimic computed tomography (CT) sign of cerebral venous thrombosis.
Keywords
Introduction
Stroke is a common presentation in emergency department but rarely seen in pediatric patients. The management is different from that of adult ischemic stroke where thrombolysis is a good optional therapy.
Cardiac disorders, identified in up to 50% of strokes in case series, are the most common risk factor for stroke in children [1]. In the canadian pediatric ischemic stroke registry (cpisr) [2], cardiac disease was identified in 25% of children with (Arterial Ischamic Stroke) (AIS). Cardiac disorders were the most common risk factor among children hospitalized with AIS in the united states from 1979 to 2000 (27% of all cases) [3].
Several cardiac disorders are associated with stroke in children: congenital heart disease, intracardiac defects, cardiac procedures,and acquired heart disease. Cardiac disorders can lead to the development of intracardiac thrombi that may symbolize to the brain or can lead to thrombosis in cyanotic patients with anemia [4]. Congenital heart disease (CHD) CYANOTIC HEART DISEASE was the most common risk factor among children hospitalized with stroke [5]. The incidence of CHD is one per 125 live births [6]. In the United States, early treatment and improved surgical techniques for cardiac disorders have increased survival rates and reduced cerebrovascular events [7]. The percentage of ischemic strokes due to cardiac disorders decreased 76% among children hospitalized with ischemic stroke between the years 1979 and 2000 [3]. The risk of stroke in children with CHD is related to the underlying abnormality, diagnostic and surgical procedures, and associated genetic or acquired factors that predispose children to thrombosis.
Cerebral venous thrombosis (CVT) is defined as an acute onset of systemic or focal neurologic symptoms consistent with cerebral venous thrombosis and neuroimaging evidence of thrombosis within cerebral veins or venous sinuses. CVT produces an obstruction of venous drainage that can lead to increased venous pressure, increased intracranial pressure, cerebral edema, hemorrhage, and venous infarction [7]. The incidence of CVT in children is estimated at 0.4 to 0.6 per 100,000 children per year and is highest in the 1st year of life.
Case Report
We present a case of Term baby, 28days old Filipino baby had history of fever for 5 days after delivery and lethargy, irritability, poor feeding associated with cyanotic spell, apnea for few seconds. Admitted to PICU connected to CPAP, treated as? sepsis antibiotic coverage after sepsis work up done including CBC, Blood culture and Urine analysis and c/s and CSF analysis, C/S, as she had cyanotic spell during his illness chest x-ray (Picture 1) and Echocardiogram was requested although this can be a part of sepsis presentation. Echo showed D-TGA, mid muscular VSD, small ASD secondum (Figure 1) so Balloon atrial septostomy procedure was done and prostaglandin treatment was started and patient show some improvement, cyanotic spell was less with other supportive mangment (IV fluid, antibiotics, still CPAP). All her cultures was negative, and clinically was stable start on oral feeding. Clinical examination was normal growth parameter (HC 35 cmHt, wt:4.5kg), no dysmorphic feature, no facial asymmetry, clear air entry, cardiac: first and second heart sound was normal, with ejection systolic murmur at left sternal area with no heaving or thrill. No organomegaly, normal neurological examination a part of mild lethargic, inactive on admission).

Picture 1: Chect x ray.
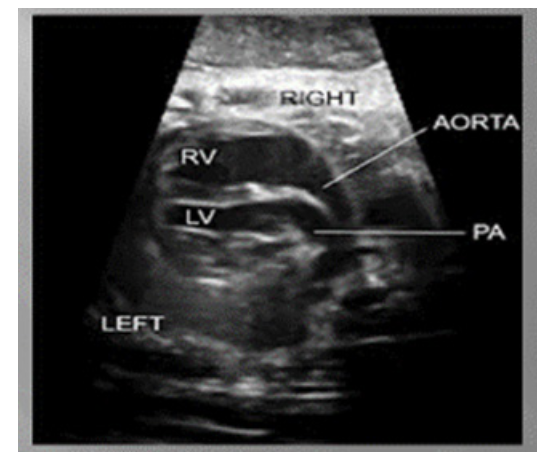
Posterior pulmonary artery and anterior aorta aligned rather than in the usual crossing arrangement.
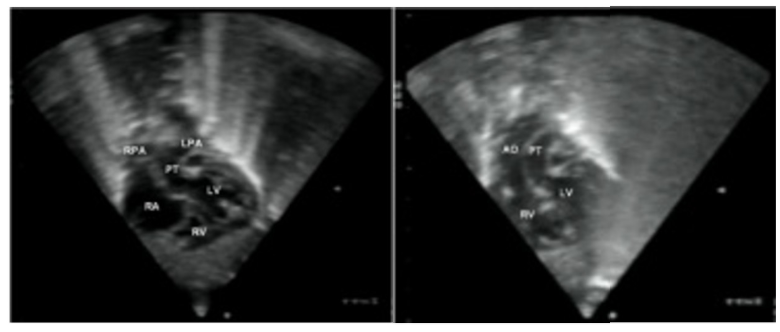
Aorta is anterior and on the right of pulmonary artery.
After improvement pt was shifted to SCU (Special Care Unit), after 3 days she develops seizures, in term of clonic jerk movement of both arm and legs for few second aborted spontaneously, was frequent with no vital sign changes. Neurology consultation done started on phenobarbitone, EEG done showed: slow posterior dominant rhythm and few intermittent sharp waves at frontocentral region. CT brain requested figure 2.
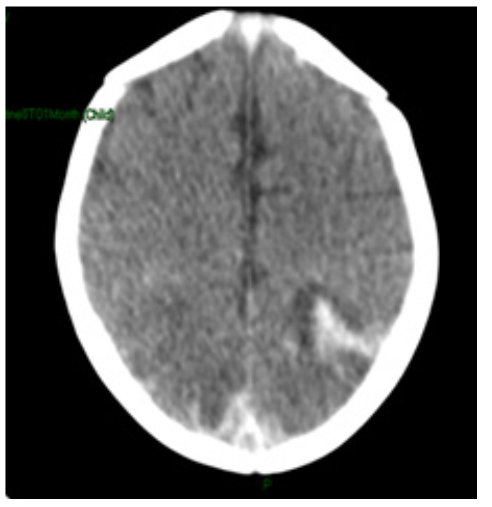
Figure 2: CT Brain w/o Contrast: Limited study due to artifact.
There is acute hyperdense hemorrhage seen in the left parietal region with surrounding hypodense edema. There is suspected right subarachnoid hemorrhage. There is hyperdensity seen in the region of superior sagital sinus, for further assessment by MRI. The ventricles are within normal.
Pt was started on heparin according to protocol after hematology consultation with daily ultrasound and APTT INR PT monitoring. After 5 days heparin was changed to enoxaprin neurology consultation was repeated they advise to continue phenobarbitone follow up in neurology clinic after 4weeks. Now patient is fit free on demand feed hemodynamically stable. On discharge patient was stable, normal feeding, no seizure or cyanotic spell, normal neurological examination no clear motor deficit.
Patient need higher cardiac center for surgical repair of D-TGA as this facility is not available in our hospital acceptable O2 saturation more than 70% demand feed baby was discharged on phenobarbitone 15mg once daily ferrous sulphate 0.4ml orally, enxoparin 4.5mg sub cutaneous every 12 hourly.
Discussion
Stroke and brain abscess are the most common neurological complications of uncorrected congenital heart disease [8].
Stroke due to cerebral arterial thrombosis has been attributed to the secondary erythrocytosis of cyanotic heart disease, which is pathologically different from primary erythrocytosis of polycythemia vera. An association between elevated hematocrit and thrombosis has been established in polycythemia vera. However, no association has been established between elevated hematocrit and secondary erythrocytosis in case of cyanotic heart disease [5].
This is not was seen in our case, but we do think that dehydration and sepsis can increase the risk of stroke with the presence cyanotic heart disease.
In addition to issues of timing, multiple mechanisms have been identified that may contribute to the These can be broadly characterized as the following: global hypoxia; global or focal ischemia/reperfusion (including hemorrhage); in-flammatory; and developmental high frequency of abnormal neurodevelopmental outcomes observed in infants with CHD [9]. Diagnostic imaging procedures for CVT include MRI, MR venography (MRV), digital subtraction angiography, CT, and ultrasonography. Conventional T1 and T2 weighted MRI with MRV is the current recommendation for the diagnosis of CVT in children. Similar to our case was diagnosed initially buy CT brain then MRI done as shown in Figure 2. If MRI is unavailable or not possible for a sick child, multi-slice CT with CT venography should be considered and is comparable with gadolinium enhanced MRV. Ultrasonography is typically employed in neonates and is most useful for detecting decreased or absent flow in the superior sagittal sinus [7].
There are no established guidelines for the treatment of CVT in children. Infection, fever, dehydration, and seizures, along with other underlying risk factors, should be treated aggressively. Anticoagulation is recommended for CVT in adults and may be indicated for use in children [10]. Thrombolytic therapy has been recommended for children with CVT who progressively worsen despite adequate anticoagulation, however in our patient was recommend by hematology to avoid the risk of recurrent seizure although there was partial ischemic changes in MRI brain and there might be risk of bleeding, in or patient the response was excellent and patient transfer to higher center for surgery and had good outcome. Exonaprin was discontinue after 3 months and repeated MRV and MRI was normal apart slight ischemic changes was seen in same area in the (Figure 3).
The clinical presentation of stroke varies according to age and location, and may be subtle. Ischemic stroke is probably more common than hemorrhagic stroke in children, but this has not been confirmed in all studies. Several risk factors for stroke in children have been reported, but frequently no cause is identified. Recent improvements in neuroimaging have contributed to a better understanding of the underlying mechanisms of stroke in children, but much work remains. In conclusion, untreated Cyanotic heart lesions not only increase the risk of cerebral infarction, but can also mimic computed tomography (CT) sign of cerebral venous thrombosis with good outcome.
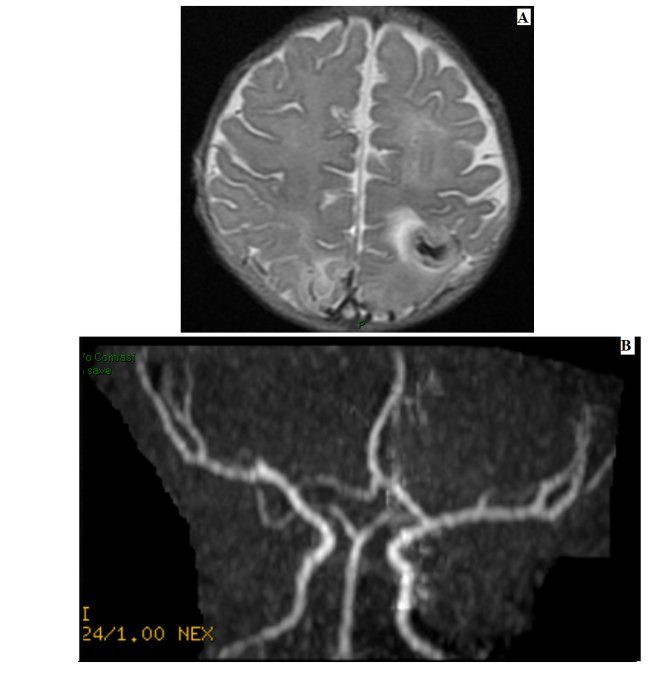
Figure 3: Brain MRI without IV Contrast administration with MRV and MRA.
Findings
A) Left Posterior Parietal Lesion Flair Weighted with Tortuous Hyper intensity on T1 Weighted images associated with lesion involving left basal ganglia with restriction on diffusion weighted images suggesting ischemic changes with some hemorrhagic. (B) No signal flow of MRV done for this lesion suggesting severe dural sinuses thrombosis. The rest of brain parechyma is normal. Ventricles and midline structures are normal. MRA done for circle of willis shows grossly normal .
References
1. Lanska MJ, Lanska DJ, Horwitz SJ, et al. Presentation, clinical course, and outcome of childhood stroke. Pediatr Neurol. 1991; 7: 333-341.
2. De Veber G. The Canadian Ischemic Stroke Study Group: Canadian Pediatric Stroke Registry: analysis of children with arterial ischemic stroke [abstract]. Ann Neurol. 2000; 48: 526.
3. Lynch JK. The hospitalization of childhood stroke in the United States, 1979–2000 [abstract]. Stroke. 2003; 34: 51.
4. Kumar K. Neurological complications of congenital heart disease. Indian J Pediatr. 2000; 67: S15-S19.
5. Fullerton HJ, Wu YW, Zhao S, et al. Risk of stroke in children: ethnic and gender disparities. Neurology. 2003; 61: 189-194.
6. Strauss A, Toth B, Schwab B, et al. Prenatal diagnosis of congenital heart disease and neonatal outcome-a six years’ experience. Eur J Med Res. 2001; 6 66-70.
7. Mahle WT, Tavani F, Zimmerman RA, et al. An MRI study of neurological injury before and after congenital heart surgery. Circulation. 2002; 106: I109-I114.
8. Miller G, Mamourian AC, Tesman JR, et al. Long-term MRI changes in brain after pediatric open-heart surgery. J Child Neurol. 1994; 9: 390-397.
9. Kumar K. Neurological complications of congenital heart disease. Indian J Pediatr. 2000; 67: S15-S19.
10. Steven P. Miller, Preoperative Brain Injury in Newborns with Transposition of the Great Arteries. Ann Thorac Surg. 2004; 77: 1698-1706.
11. Paciaroni M, Palmerini F, Bogousslavsky J. Clinical presentations of cerebral vein and sinus thrombosis. Front. Neurol. Neurosci. 2008; 23: 77-88.