Chondroid Syringoma of the Vulva: Case Report and Review of the Literature
Author'(s): Marchitelli Claudia Ester1, Absi María Lucrecia2*, Sluga María Celeste3, and Wernicke Alejandra4
1Chief of Vulvar Section, Department of Gynecology, Hospital Italiano Buenos Aires, Argentina
2Fellow of Vulvar Section, Department of Gynecology, Hospital Italiano Buenos Aires, Argentina
3Vulvar Section, Department of Gynecology, Hospital Italiano Buenos Aires, Argentina
4Department of Surgical Pathology, Hospital Italiano Buenos Aires, Argentina
*Correspondence:
María Lucrecia Absi, Juramento 3060 4A, Ciudad Autónoma De Buenos Aires, Argentina, Tel: 0054-11-4786-9261; Fax: 0054-11-4553-0631; E-mail: maria.absi@hospitalitaliano.org.ar.
Received: 30 June 2017 Accepted: 04 August 2017
Citation: Mitrovic M, Vukajlovic S, Argirovic R, et al. Chondroid Syringoma of the Vulva: Case Report and Review of the Literature. Gynecol Reprod Health. 2017; 1(2): 1-3.
Abstract
Chondroid syringoma is a rare and benign tumor which usually arises in the salivary glands, most commonly the parotid gland. Its location in the vulva is extremely rare and until now, only eleven cases have been reported. It usually presents as a persistent and indolent mass. Among the reported cases, only one described an adenocarcinoma developing within a chondroid syringoma, but the remaining were benign. These tumors tend to recur when they are not widely excised with clear margins. Malignant transformation is extremely uncommon. Since there is a slight possibility of recurrence, long term follow-up is warranted. Differential diagnoses include other solid tumors of the vulva such as angiomas, fibroid tumors and lipomas among others. Definitive diagnosis is established through histopathology. We describe the diagnosis and management of one case of chondroid syringoma of the labium majora in an 84-year-old woman.
Keywords
Introduction
Chondroid syringoma is a benign and rare tumor that arises from the myoepithelial cells which are present in the cutaneous adnexa, sweat glands, Bartholin gland or accessory breast tissue [1]. Its incidence is very low, corresponding to 0.01 to 1% of primary skin tumors. The typical presentation is in young male adults and 80% are located on the head and neck, generally affecting salivary glands such as the parotid. 10% are located in the trunk and extremities. Less frequently it involves feet, axillary region, abdomen and genitals.
The vulvar location is extremely unusual, and up to the date of this publication, only eleven cases have been reported in the literature [2]. Malignant transformation is extremely uncommon. Complete resection of the lesion with clear margins and long-term follow-up is the proposed treatment to avoid recurrence [1].
Objective
To report the diagnosis and management of one case of chondroid syringoma of the vulva at the Gynecology Department of the Hospital Italiano in Buenos Aires.
Case report
An 84-year-old woman, gravida 2, para 2, presented at the Hospital Italiano in Buenos Aires for evaluation. She complained of a palpable vulvar tumor in her right labia majora which had developed over the past year, which increased in size and generated discomfort. She only had a personal history of colon cancer.
Physical examination revealed a tumor of approximately 5-6 centimeters in the right labia majora. It was not fixed to deep tissue, and it had varicose veins on the surface as well as a hard consistency (Figure 1).

Figure 1: Vulvar tumor on right labia majora of 5-6 centimeters, mobile, with a visible varicose field.
Doppler ultrasound informed a tumor of 50 x 30 x 37 millimeters, of mixed appearance and well-defined edges, with multiple hypoechogenic cystic areas with dense content as well as a solid central hyperechogenic area. Doppler flow examination was positive. The report informed a tumor of the Bartholin gland. However, given the location and clinical presentation, this diagnosis was immediately ruled out.
Complete excision of the tumor was performed without complications. The patient was discharged 24 hours later and continued her follow up appointments to our department yearly. She remains without recurrence to date (Figures 2 and 3).

Figure 2: Complete excision of the vulvar tumor.

Figure 3: Nodular piece of 4 x 3,3 x 1,5 centimeters with a multilobulated outer surface.
The pathology report informed: Histopathology (macroscopic) showed a nodular piece of white tissue of 4 x 3,3 x 1,5 centimeters with a multilobulated outer surface. A cystic-solid tumor is recognized at cross section. The solid component is white with brown areas of myxoid morphology (Figure 4).
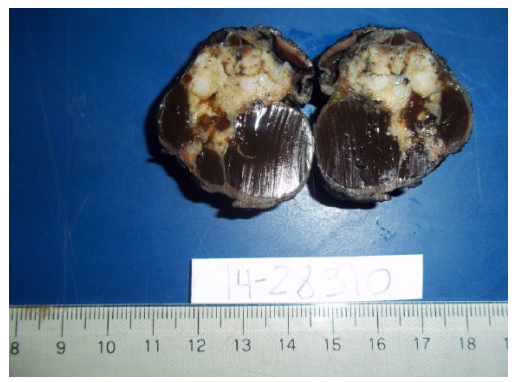
Figure 4: Macroscopy: cystic-solid tumor.
Histology: Nodular lesion with well-defined borders, constituted by tubular structures with dilated lumen containing foamy cells (macrophages) as well as papillary elements formed by cubic cells with round nuclei and eosinophilic cytoplasm, set in a fibrous matrix with areas of chondroid differentiation. Surgical margins were negative (Figure 5).
Diagnosis: Benign mixed tumor of the vulva with chondroid differentiation (chondroid syringoma of the vulva).
Discussion
Chondroid syringoma are small benign tumors, usually located on the head and neck. They are also known as benign mixed tumors or pleomorphic adenoma. The vulvar location is very rare. It has been suggested that they may arise from Bartholin glands or other glands such as vestibular, sudoriparous or mammary-like [3]. They are usually slow growing, painless, solitary tumors of less than 3 centimeters. They present as well defined, solid ovoid or round masses and are often encapsulated. Most of the cases of vulvar localization have been reported in postmenopausal women, usually located on the labia majora, without evidence of pre- existing lesions [3]. Because of the unusual localization in the genital area, the treatment modality derives from experience with pleomorphic adenoma of other localizations.
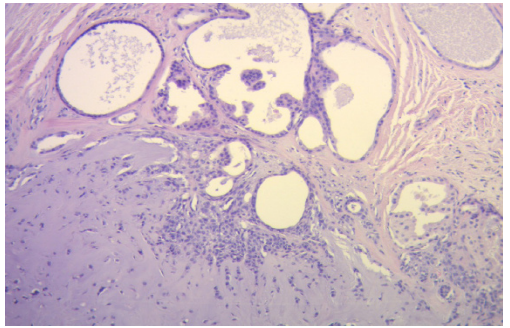
Figure 5: Microscopy: fibrous matrix with areas of chondroid differentiation.
Histopathological examination of these tumors finds epithelial and myoepithelial cells in association with myxoid or cartilaginous structures. The epithelial component shows a variety of cell types and can establish tubules, ducts, trabeculae. The stromal component can be mucoid, myxoid, chondroid or ossified [3].
Only 11 cases of chondroid syringoma of the vulva have previously been reported in the literature [4], and just one of them presented malignant transformation. In this last case, treatment consisted of wide local excision and bilateral inguinal lymphadenectomy [5].
The differential diagnoses are other solid tumors of the vulva such as angiomas, endometriomas, fibroids, lipomas, hidradenoma papilliferum and nevus, among others [6].
Conclusion
In conclusion, vulvar chondroid syringoma is a benign tumor of chronic and painless evolution. Standard treatment consists of complete excision with clear margins to reduce the possibility of recurrence. Histopathologic specimen examination is warranted in order to rule out malignancy.
References
- Dykgraaf RH, van Veen MM, van Bekkum- De Jonge EE, et al. Pleomorphic adenoma of the vulva: a review illustrated by a clinical International Journal of Gynecological cancer. 2006; 16: 920- 923.
- Su A, Apple SK, Moatmed NA. Pleomorphic adenoma of the vulva, clinical reminder of a rare Rare Tumors. 2012; 4: e16.
- Mora CA, Lara Torres HR, Ysita Morales A. Siringoma condroide: a propósito de dos casos y revisión de la bibliografía. Revista Latinoamericana de Patología. 2010; 48: 100-104.
- Tiwana KK, Nibhoria S, Kaur H, et al. Benign Vulvar Adnexal Tumors- A 5 year study in a tertiary care hospital. Journal of Family and Reproductive 2015; 9: 199-201.
- Gemer O, Piura B, Segal S, et Adenocarcinoma Arising in a Chondroid Syringoma of Vulva. International Journal of Gynecological Pathology. 2003; 22: 398-400.
- Rorat E, Wallach RC. Mixed Tumors of the Vulva: clinical outcome and pathology. International Journal of Gynecological Pathology. 1984; 3: 323-328.