Does a Second Stage Cesarean Section Increase the Risk of Cervical Insufficiency in Future Pregnancies?
Author'(s): Ayisha Buckley MD, Gina Milone MD, Naveena Chittineedi BS, Malini D Persad MD MPH, Diana Garretto MD, and Kimberly Herrera MD*
Stony Brook Medicine, Department of Obstetrics, Gynecology,and Reproductive Medicine, HSC-T9, Rm 030, Stony Brook, NY.
*Correspondence:
Kimberly Herrera, MD, FACOG, Program Director Maternal-Fetal Medicine Fellowship, Clinical Assistant Professor, Department of Obstetrics, Gynecology, and Reproductive Medicine, Stony Brook Medicine.
Received: 29 May 2020; Accepted: 25 June 2020
Citation: Buckley A, Milone G, Chittineedi N, et al. Does a Second Stage Cesarean Section Increase the Risk of Cervical Insufficiency in Future Pregnancies?. Gynecol Reprod Health. 2020; 4(3): 1-3.
Abstract
Objective: To determine the risk of cervical insufficiency (CI) in women with a history of a 2nd stage cesarean delivery (CD), and determine characteristics associated with CI with a prior CD.
Study Design: Case controlled study 1/2013 – 6/2016. ICD codes were used to identify cases with a history of CD, followed by CI in a subsequent pregnancy. Controls were patients who had a prior CD without CI. Parametric and non-parametric statistics were used; p value <0.05 was statistically significant.
Results: Of 2,000 charts, there were 15 cases (10 2nd stage, 5 1st stage). Women with a prior CD in the 2nd stage had higher odds of having CI compared to those who did not (OR 6.5 [CI 2.2-21.5], p<0.05).
Conclusion: Among those with CI, women with a prior 2nd stage cesarean delivery may be at greater risk of cervical insufficiency compared to those who do not.
Keywords
Introduction
Prematurely born infants have an increased risk of mortality and morbidity, with an inverse relationship noted with gestational age. Therefore, there has been a recent push among providers to better understand the processes of preterm birth (PTB) and how to manage and prevent it from occurring.
Cervical insufficiency (CI), defined as painless cervical dilation resulting in pregnancy loss is an important cause of PTB. The risk factors for CI can be categorized into congenital and acquired. More recent studies have shown that prior precipitous delivery and prolonged second stage of labor are associated with CI in subsequent pregnancy after prior full-term delivery; these factors may contribute to dysfunction of the cervix [1,2]. Additionally, women who have had a prior CD may impose damage to the cervix, particularly if there is a prolonged second stage of labor or cervical laceration during surgery.
Therefore, we hypothesize that women with a prior cesarean delivery (CD) in the second stage will have a higher risk of CI in the subsequent pregnancy compared to women with CDs in the first stage. We sought to determine the risk of CI in a pregnancy with a history of prior CD in 2nd stage.
Methods
This was a case-controlled study conducted via medical record review from 1/2013 to 6/2016 at an academic medical center. The study was approved by the Institutional Review Board (#934896- 4). ICD-9 and ICD-10 codes for cerclage, short cervix, and/ or history of second trimester loss were used to identify women with a history of CD in prior pregnancy and cervical insufficiency in a subsequent pregnancy (index pregnancy had to be at our institution). Controls were patients who had a prior CD without CI. Exclusion criteria included women with multiple gestations, history of preterm birth prior to, or, at the time of cesarean delivery, or incomplete medical records. The 1st stage of labor was defined as <10cm cervical dilation, whereas the 2nd stage of labor was >10cm cervical dilation. The groups were defined as cases (CD with subsequent CI) vs. controls (CD without subsequent CI). Maternal, fetal, and neonatal characteristics were collected from the electronic medical record.
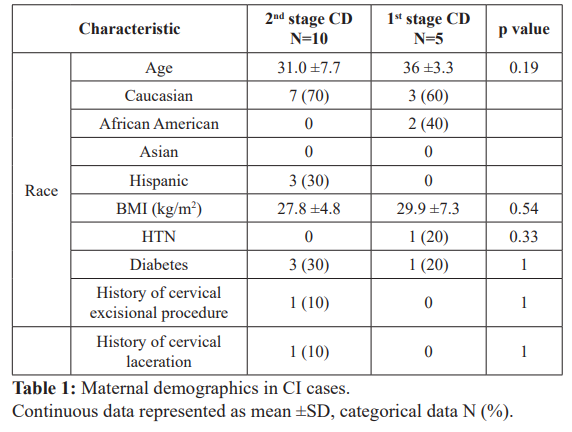
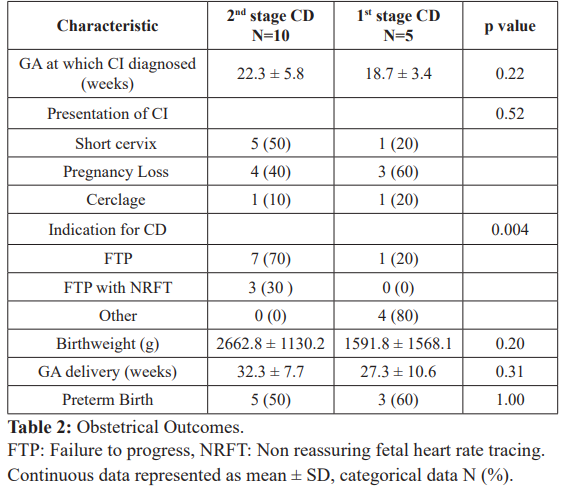
The primary outcome was the risk of having CI after a CD in the 2nd stage of labor. Secondary outcomes included maternal demographics (age, race, body mass index (BMI), hypertensive disorder, diabetes, history of cervical excisional procedure and/ or laceration), prior CD indications, and subsequent pregnancy outcomes (gestational age at CI, clinical presentation, birthweight, gestational age at delivery and rate of preterm birth) in women with CI after a CD.
Based on our power (80%) calculation, using an OR of 3.0 (based on data from Levine et al), and confidence interval of 95%, 35 cases and 137 controls would be needed. Parametric and non- parametric statistics were used to analyze the data, with p value <0.05 considered statistically significant.
Results
The total number of deliveries at our institution in this time frame was approximately 13,500. Two thousand charts were identified that met inclusion criteria and reviewed; after exclusion criteria were upheld, 15 (0.7%) cases and 690 controls (34.5%) were included. The odds ratio of having CI after a 2nd stage CD was 6.5 (95% CI 2.2-21.5, p<0.05). Among the cases, CI with 2nd stage CD was twice as common compared to those women with CI with a 1st stage CD (10 vs 5).
When looking at secondary outcomes, maternal demographics were similar between groups (Table 1). In regards to obstetrical outcomes, there were no differences between the groups with respect to the gestational age at presentation of CI, presentation of CI, gestational age at delivery or birth weight. Those with CI after a CD in 2nd stage were more likely to have a CD for failure to progress (N=7, 70%) when compared to CD in 1st stage (N=1, 20%); p value <0.004 (Table 2).
Discussion
From our data, we conclude that there are higher odds of CI following a CD in the second stage compared to women who had a prior CD in the first stage of labor. Regardless of prior CD stage, those women with CI, had similar baseline characteristics and outcomes; except those women with a prior second stage CD were more likely to have the CD due to failure to progress.
PTB is defined as birth less than 37 weeks gestation. The rate of PTB has slightly decreased from 11.99% in 2010 to 11.72% in 2011 [3,4]. The etiology of PTB is diverse, with approximately 1/3 due to preterm premature rupture of membranes (PPROM), 1/3 due to preterm labor, 1/6 due to infectious processes, and the remaining cases due to iatrogenic causes (maternal and fetal indications) [5]. Cervical insufficiency (CI), defined as painless cervical dilation resulting in pregnancy loss, does not fit into any of the above categories per se, but is an important cause of PTB. Physiologically, the cervix preserves a protective and structural barrier between the intra and extra uterine worlds by maintaining its tensile strength. As pregnancy progresses and delivery approaches, the cervix undergoes remodeling of its collagen component, which includes softening, ripening, effacement, and dilation [6]. Pathologic cervical insufficiency can be due to congenital and acquired causes. Congenital factors include collagen disorders such as Ehler’s-Danlos, uterine malformations, and now infrequently found, diethylstilbestrol (DES) exposure causing uterine and cervical malformations. Acquired risk factors include cervical trauma from prior delivery (i.e. cervical laceration), multiple mechanical dilations of the cervical canal from gynecological procedures such as dilation and curettage and/or evacuation, and prior cervical surgery for dysplasia such as cold knife cone biopsy and loop electrosurgical excision procedure (LEEP).
We theorize that in those women who have a second stage cesarean delivery (CD), there may be imposed damage to the cervical stroma that could cause CI and preterm birth. More recently, Levine et al [2], looked at the role of stage of labor of a primary CD and the risk of PTB in the subsequent pregnancy. They found that women with a second stage CD had a higher rate of spontaneous preterm delivery compared to women with a first stage CD. However, their primary outcome was overall rate of PTB as defined as preterm labor and delivery or preterm premature rupture of membranes (PPROM), and did not specify if CI occurred. This is important to note because management in a subsequent pregnancy can be altered based on this history. For example, if the patient had CI, she would be a candidate for history indicated cerclage; or if the patient had PPROM, she would be a candidate for progesterone supplementation. This would also lead to increased cervical surveillance which can help screen for CI.
One of the strengths of the study is that it is the first study to date looking at prior CD and risk of CI specifically in a large, diverse patient population. By default because our data is retrospective there are biases noted and several limitations. For one, given the study design, there is a risk of selection bias. A randomized control trial could ultimately remedy the effect of this. Additionally, we have a small number of patients that were included which is hard to draw general conclusions from. Finally, given the rarity of this event, the initial number of cases and controls calculated for the power analysis was unable to be achieved.
In summary, women with a prior CD in the second stage of labor are at a higher risk of CI in the subsequent pregnancy. Further studies are needed to determine if additional cervical surveillance is warranted in this patient population to help prevent complications.
Acknowledgments
Thank you to Stony Brook University Hospital OB/GYN department for their support.
References
- Vyas NA, Vink JS, Ghidini A, et al. Risk factors for cervical insufficiency after term delivery. Am J Obstet Gynec. 2006; 195: 787-791.
- Levine LD, Sammuel MD, Hirshberg A, et al. Does stage of labor at time of cesarean delivery affect risk of subsequent preterm birth? Am J Obstet Gynec. 2015; 212: 360.e1-7.
- Martin JA, Hamilton BE, Ventura SJ, et al. National Vital Statistics Reports, Births: Final Data for 2010. National vital statistics reports; Hyattsville, MD: National Center for Health Statistics. 2012; 61: 12.
- Hamilton BE, Martin JA, Ventura Births: Preliminary data for 2011. National vital statistics reports; Hyattsville, MD: National Center for Health Statistics. 2012; 61: 5.
- Esplin MS, Tracy A Manuck, Joseph Biggio, et al. The Phenotype of Spontaneous Preterm Birth: Application of a Clinical Phenotyping Am J Obstet Gynecol. 2015; 212: 487.e1-487.e11.
- Word RA, Li XH, Hnat M, et al. Dynamics of cervical remodeling during pregnancy and parturition: mechanisms and current concepts. Semin Reprod Med. 2007; 25: 69-79.