Double Gestation at Full Term on A Double-Horned Uterus: About one Case, at Polyclinique du Millénaire de Kisangani, D.R. Congo
Author(s): Ley Mutanda Basonika1, Albert Yemba2,3, Yenyi Ahuka Longombe1, Marcelle Dengo1, Richard Kabuyanga2,4, Michel Kyembwa2,4, Kasereka Muteke2,4, and Ahuka Ona Longombe5
1Polyclinique du Millénaire, Kisangani, D.R.Congo.
2Department of Gynecology and Obstetrics, University of Goma, Goma, D.R.Congo.
3Clinique Internationale de la Médecine Avancée au Kivu (CIMAK), Goma, D.R. Congo.
4North Kivu Provincial Hospital, Goma, D.R.Congo.
5Kisangani University Clinics, Kisangani, D.R.Congo
*Correspondence:
Dr. Albert Yemba Baruani Ahuka, Department of Obstetric Gynecology; Clinique Internationale de la Médecine Avancée au Kivu (CIMAK), located behind the Campus du Lac, Goma, D.R.Congo. Tel: (+243)998224113.
Received: 20 November 2020 Accepted: 03 December 2020
Citation: Basonika LM, Yemba A, Longombe YA, et al. Double Gestation at Full Term on A Double-Horned Uterus: About one Case, at Polyclinique du Millénaire de Kisangani, D.R. Congo. Gynecol Reprod Health. 2020; 4(4): 1-3.
Abstract
The incidence of congenital uterine malformations in the female population is estimated at 3-4%. The cloistered uterus is the most common uterine malformation, accounting for 30-50% of cases, followed by uterine malformations of the bicorneal uterus and unicorneal uterus types. We report one case of double gestation at term on a doublehorned uterus. This is the first case recorded at the Millennium Polyclinic and in the city of Kisangani (DR Congo); moreover, it highlights the obstetrical prognosis of women with this uterine malformation.
Keywords
Introduction
Uterine malformations are relatively frequent, affecting 3-4% of women; many of them are asymptomatic and their impact on reproduction is difficult to assess, so their detection requires a specific assessment. The most frequent uterine malformation is the Partitioned uterus, accounting for 30-50% of cases, followed by uterine malformations of the bicorneal uterus and unicorneal uterus type [1].
Exact prevalence is difficult to assess and Imagery techniques such as 3D ultrasound, 3D hysterosonography, and magnetic resonance imaging have only been available for a few years [2,3]. The double uterus is one of the least common abnormalities, estimated at 1 in 1000 women [4].
In a small number of case studies, double gestation, with each uterus occupied by one fetus, has been reported [5]. We report one case of a double gestation at term on a bicorneal uterus, with one fetus in each uterine cavity. This is the first case to be reported in the city of Kisangani (D.R. Congo).
Observation
She was a 23-year-old pregnant woman who was seen in a consultation for decreased active fetal movement. In her gynaecological-obstetrical history, it had been noted that she was a third gestational gesture, nulliparous with the notion of abortion (voluntary interruption of pregnancy) during her previous pregnancies. Her current pregnancy was estimated at 37 weeks based on the date of her last menstrual period, which was on 10/01/2019. Examination of the abdomen revealed an ovoid uterus with a long longitudinal axis, a uterine height of 40 cm, two auscultation sites located below the umbilicus and 10 cm apart (at the first site, heartbeats were perceived and regular at 148 beats per minute; at the second site, bradycardia was noted at 80 beats per minute), uterine contractions (2 to 3 contractions every 10 minutes, 45 to 60 seconds in duration).
On vaginal touch, a cervix erased and dilated to 4 cm, a water pocket forming, a mobile cephalic presentation was noted. Examination of the other devices was unremarkable. Emergency ultrasonography had shown a 37-week bi-amniotic twin pregnancy; both fetuses were in cephalic presentation, with badycardia of one of the twins at 76 beats per minute. The diagnosis of non-reassuring fetal status of one of the twins was then made and an emergency Caesarean section was decided. This revealed a monocervical bicorneal uterus (Figures 1A and 1B). From the left cavity, we had extracted by cephalic enucleation, a newborn male baby weighing 2630 g of APGAR 4 at the first minute and 6 at the fifth minute. We had noted a malformation of the equine varus clubfoot type. From the right cavity, we had also extracted by cephalic enucleation, a female newborn weighing 3000 grams of APGAR 9 at the first minute then 10 at the fifth minute, without apparent malformations. After directed delivery and uterine revision, the gestures performed were a hysterorraphy in simple overjet with 5/2 vicryl without touching the intercavitary septum, a visceral peritonization in simple overjet with 2/0 vicryl, a parietal peritonization in simple overjet with 2/0 vicryl, a fascia in simple overjet with 5/2 vicryl, a suture of the skin with Blair Donati stitches in 5/2 vicryl. Post-operatively, she was treated with uterotonics, analgesics and antibiotics. The immediate postoperative consequences were simple. The first newborn was entrusted to the neonatology department for better care. However, he died three days later. The mother and the second newborn were discharged from the clinic after 7 days. Further investigations (intravenous urography, cystoscopy) were planned in the mother for possible renal malformations and associated urinary tract.
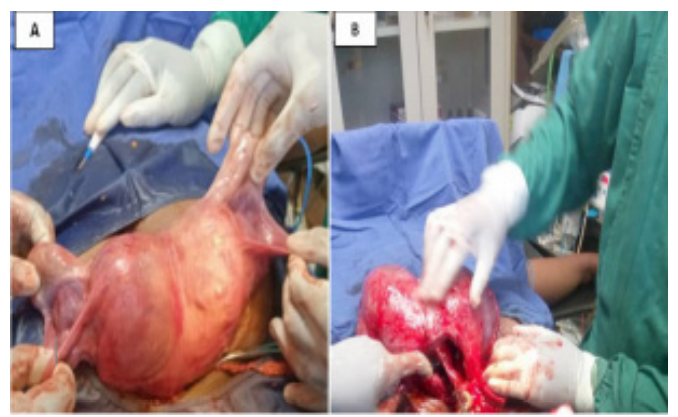
Figure 1A: Appearance of the uterus after its exteriorization, the notch of the uterine fundus is clearly visible -1B: Appearance of the uterus after fetal extraction.
Discussion
A twin pregnancy in a woman with a double uterus is an exceedingly rare event. It occurs in about one in one million pregnancies [6]. Double or duplex uteruses are the half matrices of Isidore Geoffroy Saint -Hilaire (1832), characterized by the modification of their external and internal morphology. The international classification is that of the American Fertility Society (AFS) of 1988 [7,8]. It is the most widely used in the literature. According to this classification, a distinction is made between:
- Bicervical bicorneal uterus or didelphic uterus (AFS class III) Two forms are described:
- bicervical bicervical uterus with blind hemivagina
One of the collars opens in a blind hemivagina. With menstruation, a hematocolpos with upstream hematometry appears. Study of the two renal chambers shows constant agenesis on the pathological side. Diagnosis can be made by suprapubic ultrasonography showing the bicorneal aspect of the uterine body with its two mucous membranes clearly separated; the hematometric fluid slide is clearly visible.
- permeable bicervical bicorneal uterus
It differs from the previous one by the absence of haematocolpos. The two hemi-uteruses are clearly separated, sometimes at 180° from each other. The bladder or digestive coves are visible between the two uteruses. Kidney malformations are inconsistent.
- Unicervical bicorneal uterus (AFS class IV) Two forms are described:
- the complete form: a neck, two isthmuses and two distinct cavities;
- the partial form: one neck, one isthmus and two distinct Classically, the following are described: two distinctly divergent cavities; forming an angle of more than 60°; with a distance of more than 4 cm between the horns; a notch (concavity) in the uterine fundus of more than 1 cm.
- Partitioned uteri (AFS class V)
It is the most frequent malformation, it can lead to early miscarriages by insertion of the placenta on the septum, which is classically fibrous and poorly vascularized. By the suprapubic route, the morphology of the uterus is normal. There is no notch in the fundus uteri. The uterine cavity is divided by a myometrial bridge which creates a more or less complete partition. A distinction is made between corporal, sub-total or cervical forms.
In relation to our clinical case, it was a unicervical bicorneal uterus in its complete form with a cervix, two isthmies and two distinct cavities. Each cavity was occupied by a full-term fetus. The presence of twins in each of the cavities of a double uterus was first described in 1927. To date, there are only about 20 cases of twin pregnancies on a double uterus in the medical literature. Some authors report cases of twin pregnancies on the twin uterus that did not reach term [5,6]. Claire Ross et al. report in 2017, the case of a woman carrying a full-term twin pregnancy on a bicervical twin uterus (didelphe), without any notion of PMA (medically assisted reproduction), each fetus occupying one of the uterine cavities. She will deliver two healthy newborns by Caesarean section [9]. The same was true in our clinical case, the pregnancy had come to term, and the pregnant woman had delivered by Caesarean section. The only difference was that it was a bicervical bicorneal uterus in the clinical case of Claire Rosse; whereas in our case it was a unicervical bicorneal uterus. As a result, a twin pregnancy on a bicorneal uterus can come to term, as our clinical case and that of Claire Ross et al. L′utérus bicorne complicates the pregnancy, but does not l′empêche make it possible to carry it to term [10]. C′est often the pregnancy itself that reveals the malformation because
it can cause repeated abortions, late miscarriages or premature deliveries [7,11]. It is essential to look for uterine malformation in a patient with a history of recurrent miscarriage, late miscarriage or premature delivery [12]. Our patient has no history of spontaneous abortion or premature delivery; the pregnancy progressed to 37 weeks of amenorrhea.
In our circles, the early diagnosis of a uterine malformation is difficult to establish and the obstetrical outcome remains unassessed. The difficulty stems from the fact that it is often asymptomatic and the absence of specific imaging equipment to establish the diagnosis [2,3]. Caesarean section is often the only way to make the diagnosis [13]. In our case, the diagnosis of a bicorneal uterus was per operative. Idi IY et al [14] , reported a case of uterine malformation discovered by chance during a Caesarean section. According to Roissier MC et al, it is not exceptional to make the diagnosis at the first check-up or during vaginal delivery [12].
Organogenesis of the genitourinary tract allows the interpretation and classification of genital malformations. It is done in phase. A first urinary phase, a second urinary and genital phase. The third phase is responsible for the external morphology of the genital tract and the fourth phase is that of the resorption of the wall of Muller's canals, it is responsible for the internal morphology of the genital tract. Between ten and thirteen weeks, the abnormalities observed are a defect in the fusion of the two Muller's canals, at the origin of the bicorn uterus. The malformations observed are related to the date of occurrence of the teratogen during organogenesis. Thus, after thirteen weeks, a disorder of resorption of the septum at the origin of the partitioned uterus is observed [12,13,15].
We have not repaired the malformation because for uni or bicervical bicorn uteri, surgery to reunite the two hemi-uteri, described by Strassmann in 1952 cited by Hafsa and Salim [16,17], has not shown any real benefit although the surgery is simple but reserved only for patients whose obstetrical prognosis is extremely unfavourable and whose anamnesis reveals several late miscarriages.
Conclusion
A twin pregnancy on a twinned uterus can come to term, as our clinical case shows. In our context, the detection of certain uterine malformations as well as the obstetrical outcome remains a challenge in our less equipped hospitals. This is why the diagnosis of a bicorneal uterus in our gestant was made during an intraoperative procedure. Further investigations (IVU, cystoscopy) should be carried out to look for possible kidney malformations and associated urinary tract malformations.
References
- Saravelos SH, Cocksedge K, Tin-Chiu Li. Prevalence and diagnosis of congenital uterine anomalies in women with reproductive failure: a critical Hum Reprod Update. 2008; 14: 415-429.
- Raga F, Bauset C, Remohi J, et al. Reproductive impact of congenital Mullerian anomalies. Hum Reprod. 1997; 12: 2277-2281.
- Nahum G. Uterine anomalies: How common are they, and what is their distribution among subtypes? J Reprod Med. 1998; 43: 877-887.
- Bhagavath B, Greiner E, Griffiths K, et al. Malformations utérines: une mise à jour du diagnostic, de la gestion et des résultats. Obstet Gynecol Surv. 2017; 72: 377-392.
- Heinonen P. Implications cliniques de l’utérus didelphique: suivi à long terme de 49 cas. EURJ Obstet Gynecol Reprod Biol. 2000; 91: 183-190.
- Al Yaqoubi HN, Fatema N. Successful Vaginal Delivery of Naturally Conceived Dicavitary Twin in Didelphys Uterus: A Rare Reported Case. Case Rep Obstet Gynecol. 2017.
- The American Fertility Society classifications of adnexal adhesions. Distal tubal occlusion, tubal occlusion secondary to tuballigation, tubal pregnancies, mullerian anomalies and intra uterine adhesions. FertilSteril. 1988; 49: 944-955.
- Nicolas PERROT, Isabelle FREY. Doppler-3D en gynécologie- obstétrique, 6ème édition. Elsevier Masson SAS, 2014; 292.
- Ross C, El-Hassan H, Lakasing L. Uterus didelphys: two pregnancies, two term breech caesarean BMJ Case Rep. 2018.
- Mezane S, Achenani M, Benabdeljalil Y, et al. Grossesse sur utérus bicorneun cas avec revue de la GJ Med res e Gynecol Obstet. 2014; 14: 35-38.
- Deutch T, Abuhamad A. The role of three-dimensional ultrasonography and magnetic resonance imaging in the diagnosis of mullerian duct anomalies: a review of the literature. J Ultrasound Med. 2008; 27: 413-423.
- Rossier MC, Bays V, Vial Y, et Les malformations utérines : diagnostic, pronostic et prise en charge en 2008. Rev Med Suisse. 2008; 176: 2253-2263.
- Osman A, Ihssane H, Adil C, et al. Grossesse sur utérus cloisonné menée à terme: à propos d’un cas. Pan Afr Med J. 2015; 22: 219.
- Idi IY, Mukuku O, Makinko IP, et Utérus bicorne bicervical perméable: découverte fortuite lors d’une césarienne d’urgence chez une multipare lushoise. Pan Afr Med J. 2013; 15: 75.
- Ardaens Y, Levaillant JM, Bady J, et al. Malformations utérines et du tractus génital féminin. EMC - Radiodiagnostic- Urologie-Gynécologie. 2013; 8: 1-11.
- Hafsa A, Hanane S, Saad B, et La grossesse gémellaire sur un utérus pseudo unicorne: à propos d’un cas. Pan Afr Med J. 2015; 22: 330.
- Salim R, Woelfer B, Backos M, et al. Reproductibility of three-dimensional ultrasound diagnosis of congenital uterine anomalies. Ultrasound Obstet Gynecol. 2003; 21: 578-582.