Effect of Placental Tissue Sampling Site on Placental Protein Expression Outcome
Author(s): Basu Jayasri*, Encalada Diane M, Wu Yingyi, Oraee Sara, Mishra Aruna and Mikhail Magdy
Department of Obstetrics & Gynecology, BronxCare Health System, NY, USA.
*Correspondence:
Jayasri Basu, PhD, Director - Graduate Medical Education, Department of OB/GYN, Bronx Care Health System, Clinical Assistant Professor of Obstetrics & Gynecology and Reproductive Science, Icahn School of Medicine of Mount Sinai, 1276 Fulton Avenue Room 233, Bronx, NY 10456.
Received: 13 August 2020 Accepted: 01 September 2020
Citation: Basu J, Encalada DM, Wu Y, et al. Effect of Placental Tissue Sampling Site on Placental Protein Expression Outcome. Gynecol Reprod Health. 2020; 4(4): 1-6.
Abstract
Introduction: We investigated whether placental tissue sampling site influences placental protein expression outcomes. Vascular endothelial growth factor (VEGF), VEGF165 and VEGF165b proteins were selected as candidate proteins and term delivered placentas from normotensive women was investigated.
Methods: Maternal side of each 26 placentas was divided into four quadrants: North-East quadrant was designated Q1, South-East as Q2, South-West as Q3 and North-West as Q4. Chorionic villi (CV) were isolated from placental sections of each quadrant. Pieces of CV from each quadrant were placed in separate tubes pre-labeled with placental ID and quadrant number. Tubes were stored at -80o C until assay. Monoclonal antibody based ELISA kits from R&D Systems were used to determine protein expression. The vascular pattern of each placenta was also analyzed. For statistical analysis, ANOVA and Pearson's correlation were used. P<0.05 was considered significant.
Results: Analysis of 104 CV tissues showed no difference in the expression patterns of VEGF165 and VEGF165b proteins between the four quadrants. VEGF165 and VEGF165b proteins exert opposing effects on angiogenesis, yet the two proteins were significantly correlated (r2
=0.527, p=0.0001). Dispersal type of placental vasculature was dominant compared to magistral type.
Conclusions: The study validates that VEGF165 or VEGF165b proteins expression remain unchanged irrespective of the site from where the tissues are sampled. The significant correlation between the two proteins suggests, that angiogenic modifications of placental vasculature that enables maximum blood to flow through in the third trimester of human pregnancy, is dependent on the synergistic actions of these two proteins. The existence of VEGF165b protein in amounts higher than that of VEGF165 substantiates its potential role in human pregnancy. The coexistence of VEGF165b protein in placental tissue could be a physiological phenomenon to restrain overexpression of VEGF165 during placental development, which if left unchecked, could lead to pregnancy-related complications.
Keywords
Introduction
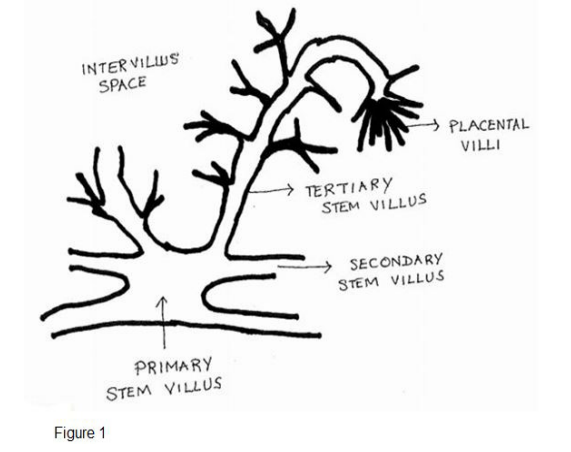
The placenta is the first fetal multifunctional organ to develop during pregnancy. Its intimate involvement with both the mother and the developing fetus throughout gestation makes it a desirable organ to study to better understand the intrauterine environment. The structure of human placenta is limited on the maternal sideby a decidual trophoblastic plate and on its fetal side by the chorionic plate. Blood vessels branching from the umbilical arteries and vein spread across the chorionic plate. A cartoon of the branching pattern of placental blood vessels is shown in Figure 1 The branching pattern of placental blood vessels has been studied by many investigators [1-3]. Romney and Reid [1] in their study report that the umbilical blood vessels branch and re-branch to form the main stem villi, the secondary villi, the tertiary villi and the placental villi. These villi lie free within the intervillous space, however, some remain adherent to decidual connective tissue and are termed the anchoring villi. Groups of these villi constitute the cotyledon, the functioning unit of the placenta. The success of any pregnancy depends on the proper development of the branching villous structure of the placenta and the network of fetal blood vessels it contains, at the initial phase of pregnancy [2]. As pregnancy advances, the vascular network within the placental villi continues to expand.
We in the past have studied the placenta. Our goal was to delineate the expression pattern of several key placental proteins throughout gestation in normal pregnancy and in preeclampsia [4-6]. For these studies, we took a section from each placenta, isolated the chorionic villi and had determined the protein expression patterns. The lingering question however that currently occupies our minds is since the placenta differs significantly in its structure and vasculature, could the tissue sampling site have influenced the placental protein expression outcomes? The vascular patterns of the placenta have been studied since the early 1900 and revealed two very distinct patterns to exist: the magistral and the dispersal type [7,8]. The noteworthy difference between the two patterns is in the magistral pattern, the umbilical vessels reach the placental margin without marked reduction in caliber; even though small vessels may branch off as the main blood vessel courses towards the placental margins. In the dispersal type, the umbilical vessels undergo successive divisions with gradually diminishing caliber towards periphery [7,8]. We therefore questioned whether the protein expression that we have reported in our previous studies 4-6] would have been different had we sampled the tissue from a different site in the same placenta? To resolve this nagging issue, we launched this study in which we compared the protein expression patterns between four different quadrants of the same placenta. We focused our attention for this study on term delivered placentas because it is in the third trimester of human pregnancy, placental vascular growth increases exponentially and fetal demands are at its peak. This we postulated will enable us to identify the difference in protein expression patterns based on placental sites. The candidate placental proteins that we selected for this investigation were vascular endothelial growth factor (VEGF)165 and VEGF165b. The reason in selecting these proteins is because placenta is a primary active site of angiogenesis; and both (VEGF)165 and VEGF165b are intimately involved in angiogenesis, but exert opposing effects [9,10].
Methods
The investigative protocol for the study was approved by the Human Subject Ethics Committee of the BronxCare Health System, New York, USA. Term delivered placentas was collected following spontaneous vaginal delivery or caesarean section within 30 minutes of the procedure. The study protocol allowed collection of the placentas following clinical assessments from women who were normotensive throughout pregnancy and had no signs of any pregnancy related abnormalities or any other medical complications; and whose placentas would otherwise had been discarded. The reasons for the caesarean section were labor dystocia and fetal malpresentation.
The method by which each placenta was processed has previously been described in details [11]. Briefly, the adhering blood clots and the placental membranes were first removed. The umbilical cord was removed as well, leaving only a short stump at the insertion point where the umbilical cord enters the placenta. The placenta was then weighed and the weight was recorded. The placenta was then placed on the table with the fetal side of the placenta appearing on top. A disposable measuring tape was placed at the bottom of the placenta to document its size, and a photograph of the placenta was taken. Each placenta was then flipped from left to right to expose the maternal side of the placenta. Each placenta was then visually dissected into four quadrants (Qs); and sections from each quadrant was removed and processed one at a time. The section taken from the north-east region of the placenta was designated Quadrant 1, south-east section was designated as Quadrant 2, south-west section was designated as Quadrant 3 and north-west section was designated as Quadrant 4.
After a segment of tissue from each placental quadrant was removed the section was thoroughly washed. The segmented tissue was further cut into smaller pieces and placed in a petri dish with normal saline. The tissue fragments were then dissected in saline to isolate free floating chorionic villi that were not anchored to the basal plate nor were emerging from the chorionic plate surface vessels. Several isolated chorionic villi tissues pieces from each placental quadrant were placed in separately labelled cryovials that bore the same placental ID and quadrant number. The remaining method how the tissue from each placental quadrant was handled and stored was similar to the method that has been described in greater details elsewhere [11]. VEGF165 and VEGF165b protein expressions were determined by commercially available enzyme- linked immunosorbent assay (ELISA) kits from R&D Systems, Minneapolis, MN. Each kit used monoclonal antibody to human protein VEGF165 or VEGF165b as the capture antibodies. A Tecan infinite 200 Pro microplate reader (Tecan Systems Inc., San Jose, CA) set at 450 nm with wavelength correction set at 540 nm was used to measure the absorbance during the ELISA assay. The manufacturer claims that the sensitivity of the ELISA assays for VEGF165 and VEGF165b protein are 31.2 pg/ml and 62.5 pg/ml, respectively.
The IRB approved protocol also allowed the collection of clinical information pertaining to the women from whom placental tissues were obtained. These included: maternal age, race/ethnicity (selfreported), gestational age (as determined by ultrasound or by initial date of the last menstrual period), last maternal systolic and diastolic blood pressure prior to term delivery and newborn's weight and sex. Tissues and clinical information gathered during sample collection were de-identified before exiting the delivery suites.
Determining the pattern of placental vasculature
The incidence of Dispersal or Magistral type of placental vasculature in our collected placentas was determined as follows. Briefly, we followed the method of Prasad et al. [7]. The diameter of the blood vessels at the insertion point (the location where the umbilical cord inserts into the placenta) was compared to the diameter of the blood vessels at the periphery. If the diameter of the vessels at the placental margins was half or less than half of that at the insertion point, then the placental vasculature was categorized as Dispersal type. However, if the diameter of the blood vessel was more than half at the placental margins compared to that of the insertion point, then the vasculature was categorized as Magistral type.
Statistical Analysis
The statistical software package SPSS, version 26 (IBM Corporation, Armonk, NY) was used for statistical analyses. One- way ANOVA and Pearson's correlation were used for analysis and the level of statistical significance was set at P<0.05.
Results and Discussion
Most of the studies on placenta are primarily geared towards understanding the intrauterine environment of a developing fetus or in understanding the various disorders of placentation. The spectrum of complications related to disorder of placentation includes late spontaneous miscarriage, abruptio placentae, fetal growth restriction, pre-term rupture of the membranes and premature delivery [12]. Since placenta is the only organ that is intimately involved with both the mother and the developing fetus throughout gestation; and the aforementioned syndromes resolves once the placenta is removed [12] hence, placenta serves as a desirable tool to carry out the studies.
Placental angiogenesis is a normal physiological process that is tightly regulated throughout pregnancy. VEGF is the first angiogenic factor that was identified [13]. Expression of VEGF correlates most closely with the spatial and temporal events of vascular growth [14]. VEGF, however, consists of at least seven structurally homologous isoforms: VEGF121, VEGF145, VEGF148, VEGF165, VEGF183, VEGF189, and VEGF206. These isoforms are produced from different splicing variants of VEGF pre-mRNA. In 2002, Bates et. al. described a novel group of VEGF splice variants which are also encoded by the VEGF gene [9]. These novel isoforms are formed by alternate splicing of the terminal exon, hence, these novel isoforms are similar in size but differ in their terminal six amino acids; and are named VEGFxxxb. VEGF165 is well recognized angiogenic molecule [9,10], however, the terminal six amino acids in novel isoform VEGF165b, formed by alternate splicing of VEGF165, confer an antiangiogenic property to it [9,10].
In the present study we did not however investigate the angiogenic or antiangiogenic property of placental VEGF. What we investigated instead was whether the expression patterns of any placental protein would vary based on the site from where the tissue was sampled, primarily because placenta differs markedly in its structure and vascular patterns. Placenta is one of the richest sources of both pro-angiogenic and anti-angiogenic molecules [9]. Additionally, in the third trimester of human pregnancy, placental vascular growth, blood flow and fetal weight increase exponentially. Hence, for this study we focused our attention on third trimester term delivered normal placentas. Regarding selecting the candidate proteins for the study, we selected VEGF165 and VEGF165b proteins. Both VEGF165 and VEGF165b proteins are generated from the same transcript, and their relative amounts in any tissue are dependent on alternative splicing [15]. It appears that VEGF165b protein is highly expressed in non-angiogenic tissues, and in contrast with VEGF165 is downregulated in tumors and other pathologies associated with abnormal neovascularization [15].
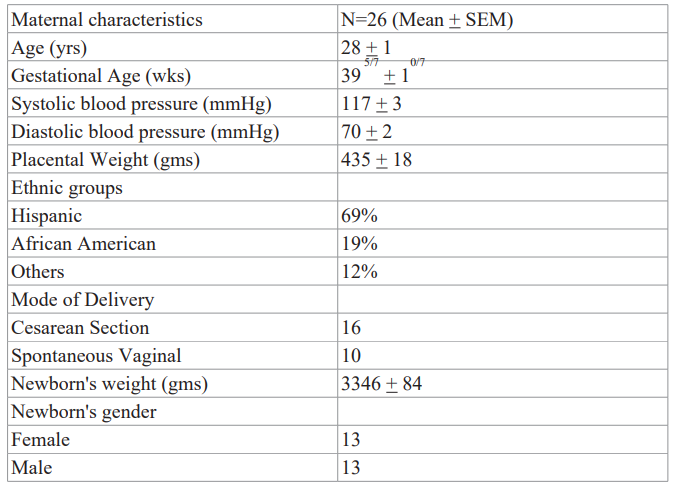
Table 1: Clinical characteristics of women from whom placentas were obtained.
The clinical characteristics of the women from whom placentas were taken are presented in Table 1. All women were normotensive. The mean maternal age was 28 ± 1 years. The average gestational age was 395/7 ± 10/7 weeks. Self-reported race/ethnicity showed 69% of the women were of Hispanic origin, 11% were of African American origin and remaining was of other ethnic groups. A total of 16 women delivered by C-section and the remaining 10 women delivered vaginally. Information on the gender of newborns showed that 13 were females and 13 were males. The last recorded systolic and diastolic blood pressures of the women prior to their delivery were collected, and the average systolic and diastolic blood pressure of the women from whom placental samples were collected was 117 ± 3 and 70 ± 2 mm Hg, respectively.
In this study, chorionic villi protein expression of VEGF165 and VEGF165b protein were primarily compared between four different quadrants of each placenta. A total of 26 term delivered placentas were collected from women who were normotensive throughout pregnancy and did not have any other medical complications. Protein expressions of 104 chorionic villi samples obtained from four different quadrants of each of 26 normal placentas were analyzed for both VEGF165 and VEGF165b proteins by Direct Sandwich ELISA method. The intra-assay and inter-assay variations for the assays were between 8-12%. Even though the 26 placentas collected for the study differed significantly in their structure and vascular patterns (Figure 2), statistical analysis by ANOVA revealed that placental VEGF165 and VEGF165b proteins both were expressed equally in all four quadrants of the placenta (Table 2). Our findings confirm that placental VEGF165 and VEGF165b proteins remain equally expressed irrespective of the site from where the tissues were sampled. Figure 2 depicts the vascular pattern of all 26 placentas collected for the study. The incidence of dispersal pattern was 58%, comparatively higher than the Magistral type (42%). The higher incidence of the dispersal pattern of placental vasculature is consistent with the results reported by other investigators (7, 8). In this study, we did not see any difference in placental VEGF165 and VEGF165b protein expression based on a) placental vascular pattern, b) ethnicity of the women from whom placentas were collected (Hispanic vs Black), c) method of delivery either spontaneous vaginal delivery or cesarean section or d) sex of the newborn the mother was carrying. Placental VEGF165 and VEGF165b proteins ranged widely between placentas. VEGF165 ranged from 123 – 411 pg/100 mg tissues; while VEGF165b protein ranged from 99 -1269 pg/100 mg tissue. The two scatter plots (Figures 3 and 4) demonstrate, however, that higher placental expression of placental VEGF165 or VEGF165b proteins does not necessarily correspond to greater placental weight. Rather placental weight was found to be comparatively lower when either VEGF165 or VEGF165b protein expression was above the mid ranges. The relationship between higher levels of VEGF165 or VEGF165b proteins expression and placental weight deserves further investigation. The other results of the study include: Positive correlations seen between placental length and placental weight (r2 = +0.389, p= 0.05); and between placental weight and newborn weight (r2 =+0.792, p=0.0001)
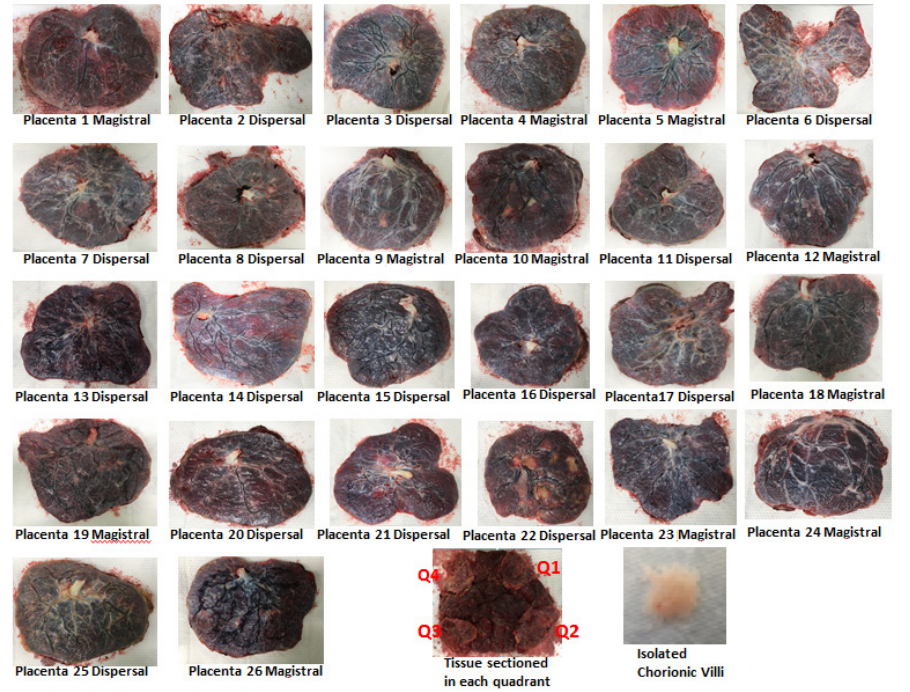
Figure 2. Placental vasculature of the 26 placentas collected for the study. The second last image at the bottom shows the maternal side of a placenta and how sections were taken from each placental quadrant.
The bottom last image depicts isolated chorionic villi in normal saline in a petri dish.
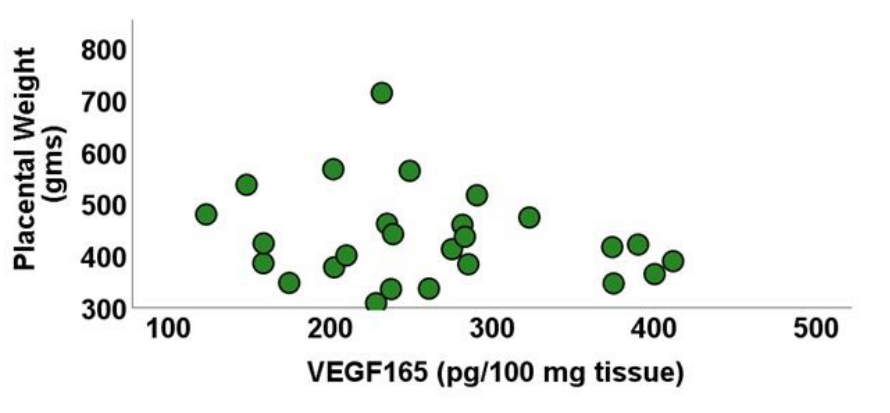
Figure 3:Correlation between placental weight and chorionic villi VEGF165 protein.
VEGF: Vascular endothelial growth factor
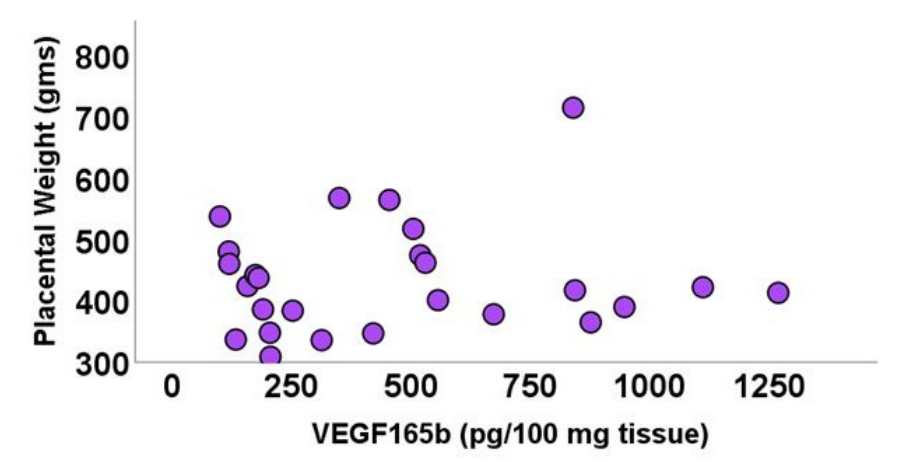
Figure 4. Correlation between placental weight and chorionic villi VEGF165b protein.
VEGF: Vascular endothelial growth factor
Results of our study showed that of the two VEGF isoforms, protein expression of VEGF165b in term delivered placental tissues was higher than that of VEGF165 (Table 2). To our knowledge there is only one other study cited in the literature reported by Bates et al. [9] in which human placental VEGF165b protein concentration is reported to be significantly lower than that of VEGF165. The placentas selected for the Bates et al. study were taken from healthy normotensive pregnant women after caesarean section for a variety of reasons, including fetal distress, failure to progress and placental abruption. In our study, we have collected placentas from women at term who were normotensive throughout pregnancy. Of the 26 placentas that were collected for this study, 10 of the placentas were delivered vaginally and 16 were delivered by caesarean sections. The primary reasons for the caesarean sections were labor dystocia and fetal malpresentation. In our study, method of delivery did not have any impact on the placental expression of VEGF165 or VEGF165b proteins.
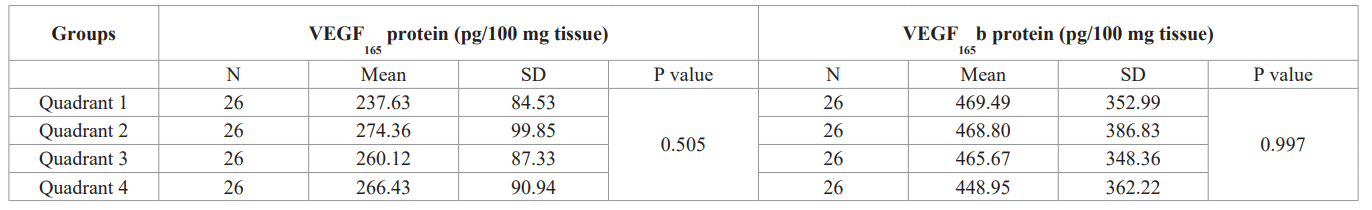
Table 2: Chorionic villi expression of VEGF165 and VEGF165b proteins in placental quadrants. By ANOVA
The 26 women from whom term delivered placental tissues were collected were all normotensive throughout gestation. The last recorded systolic and diastolic blood pressures of the women prior to their delivery were collected for the study. Pearson's correlation results showed that maternal systolic and diastolic blood pressure were significantly correlated (r2=0.552, p=0.003). The significant positive correlation between systolic and diastolic blood pressure of these women substantiates that these women were normotensive. It also corroborates that an adequate placental blood flow existed in the third trimester of pregnancy keeping in pace with increased fetal growth; and was perhaps the reason why the outcomes of these pregnancies were all healthy, normal newborns. Even then an interesting finding emerged from this study. Pearson's correlation results revealed that the placental length was inversely correlated to diastolic blood pressure of the mother (r2=0.522, p=0.006). At this point we are unable to explain the significance of our finding.
Pearson's correlation results of this study also revealed a significant correlation between placental VEGF165 or VEGF165b proteins (r2=0.527, p=0.001) consistent with the results reported by Bates et al. [9]. In our previous report, similar significant correlation (r2 =0.271, p= 0.033) was seen between the two isoforms of VEGF in the third trimester of human pregnancy [4,16]. Based on the persistent presence of VEGF165b protein throughout gestation as seen in our previous study [16] we suggest that VEGF165b protein in human pregnancy must play a significant role. We additionally postulate that in the third trimester of human pregnancy, both
Conclusions
The study primarily validates that even though the placenta differs significantly in its structure and vasculature, VEGF165 or VEGF165b proteins are equally expressed in normal human term delivered placenta, irrespective of the site from where the tissues were sampled or the vascular pattern of the placenta. Our data substantiates that VEGF165b proteins plays a significant role in human pregnancy. We hypothesize that coexistence of VEGF165b protein along with VEGF165 protein in placental tissue could be a physiological phenomenon to restrain overexpression of VEGF165 during placental development, which if left unchecked, could lead to pregnancy-related complications.
Acknowledgements
The study was funded by the Residency Program of the BronxCare Health System. The authors thank the staff members of the Department of Obstetrics & Gynecology at BronxCare Health System for their support in carrying out this study.
References
- Romney SL, Reid DE. Observations on the fetal aspects of placental circulation. Am J Obstet Gynecol. 1951; 61: 83-98.
- Boss AL, Chamley LW, James Placental formation in early pregnancy: how is the center of the placenta made? Human Reprod Update. 2018; 24: 750-760.
- Boyd JD, Hamilton WJ. The human placenta Cambridge. Heffer. 1970.
- Basu J, Gonzalez S, Banajjar V, et al. Comparative study of chorionic villi protein expression between normotensive pregnancy and EC Gynaecology. 2019; 8: 943-956.
- Basu J, Seeraj V, Gonzalez S, et al. Correlation between placental matrix metalloproteinase-9 and tumor necrosis factor-α protein expression throughout gestation in normal human pregnancy. J Clin Obstet Gynecol & Infertil. 2017; 1: 1-6.
- Basu J, Agamasu E, Bendek B, et al. Correlation between placental matrix metalloproteinase-9 and tumor necrosis factor-α protein expression throughout gestation in normal human pregnancy. Reprod Sci. 2018; 25: 621-627.
- Cunnigham FG, Gant NF, Lenevo KJ, et Physiology of pregnancy, Placenta and foetal membranes. Williams Obstetrics 21st ed. New York, McGraw Hill Inc. 2001; 109- 128.
- Bates DO, MacMillan PP, Manjaly JG, et The endogenous antiangiogenic family of splice variants of VEGF, VEGFxxxb, are down-regulated in preeclamptic placentae at term. Clin Sci (Lond). 2006; 110: 575-585.
- Pritchard-Jones RO, Dunn DB, Qiu Y, et al. Expression of VEGF(xxx)b, the inhibitory isoforms of VEGF, in malignant melanoma. Br J Cancer. 2007; 97: 223-230.
- Basu J, Oraee S, Wu Y, et Regional variations in placental protein expression of matrix metalloproteinase-9 in term uncomplicated pregnancy. EC Gynaecology. 2020; 9: 26-33.
- Bronsen I, Pijnenborg R, Vercruysse L, et al. The "Great obstetrical syndromes" are associated with disorders of deep placentation. Am J Obstet Gynecol. 2011; 204: 193-201.
- Senger DR, Galli SJ, Dvorak AM, et al. Tumor cells secrete a vascular permeability factor that promotes accumulation of ascites fluid. Science. 1983; 219: 983-985.
- Keck PJ, Hauser SD, Krivi G, et al. Vascular permeability factor, an endothelial cell mitogen related to PDGF. Science. 1989; 246: 1309-1312.
- Peiris-Pagès M. The role of VEGF165b in pathophysiology. Cell Adhesion & Migration. 2012; 6: 561-568.
- Basu J, Gonzalez-Ramos S, Banajjar V, et al. Chorionic villi expression of two vascular endothelial growth factor proteins in normal human Integr Gyn Obstet J. 2018; 1: 1-6.