Effective and Efficient Approach to Cervical Cancer Screening Education in Ethiopia
Author'(s): Gossa Weyinshet1,2*, Melaku Mesfin3, Klyushnenkova Elena1, Nigatu Balkachew4, Bekele Delayehu4 and Khanna Niharika1
1University of Maryland, Department of Family and Community Medicine, US.
2University of Michigan, Department of Family Medicine, US.
3Eastern Michigan University, US.
4Saint Paul's Hospital Millennium Medical College, Department of Obstetrics and Gynecology, Ethiopia.
*Correspondence:
Weyinshet Gossa MD, University of Maryland, Department of Family and Community Medicine, US, Tel: 667-214-1812; Fax: 410-685-1973; E-mail: wgossa@gmail.com.
Received: 20 August 2017 Accepted: 19 September 2017
Citation: Weyinshet G, Mesfin M, Elena K, et al. Effective and Efficient Approach to Cervical Cancer Screening Education in Ethiopia. Gynecol Reprod Health. 2017; 1(3): 1-6.
Abstract
Objectives: Cervical cancer is the second most common cancer and the leading cause of cancer related deaths among women in Ethiopia, however, cervical cancer screening is almost nonexistent. This study provided training and assessed knowledge and clinical skills of cervical cancer screening among medical students at Saint Paul Hospital and Millennium Medical College (SPHMMC) in Ethiopia.
Methods: This study consisted of training on cervical cancer screening and assessment of knowledge and clinical skills of cervical cancer screening using pre and post surveys. Subjects were medical students in years 4(M4), 5(M5) and 6(M6) at SPHMMC. Analysis consisted of calculating survey scores.
Results: Participants (N=28) were 21 males and 7 females. Knowledge assessment median scores were 55.9% pre-training and 75.0% post-training (Wilcoxon signed rank test p=0.001). Baseline experience with speculum examination and Visual Inspection with Acetic acid (VIA) were low. Pre-training, 75% were familiar with “acetowhite epithelium” and its significance versus 95.5% post-training (McNemar’s binomial test p ≤ 0.1). Some level of comfort in identifying aceto-white changes was 52% pre-training and 82% post-training (McNemar’s binomial test p<0.05). Some level of comfort in identifying mosaicism and punctation was 48% pre-training and 70% posttraining (statistically not significant).
Conclusions: There is significant gap in knowledge and limited basic clinical skills of cervical cancer screening among Ethiopian medical students. It is possible to achieve significant improvement in knowledge and clinical skills of cervical cancer screening with short educational intervention. Similar educational intervention should be provided to health care providers in Ethiopia to enhance cervical cancer screening.
Keywords
Introduction
Cervical cancer rate has significantly declined in the developed world while it remains very high in developing countries. Cervical cancer is the fourth most common cancer and the seventh most common cancer overall worldwide. In 2012, there were estimated 528,000 cases and 266,000 deaths from cervical cancer worldwide. Estimated 85% of the cervical cancer and 87% of cervical cancer deaths occur in developing countries. Cervical cancer is the most common cancer among women in eastern and central Africa [1]. Despite high rates of cervical cancer in developing countries, screening rates are poor; 19% on average and range from less than 1% to 75% [2].
Ethiopia is a developing country with one of the poorest cervical cancer screening rates. There are 29 million women 15 years and older at risk of developing cervical cancer in Ethiopia. Cervical cancer is the second leading cause of cancer among all women and the leading cause of cancer related deaths among women 15 to 44 years old in Ethiopia. Estimated 7, 095 cervical cancer cases and 4, 732 cervical cancer deaths occur annually. However, only 0.8% of women ages 25 to 64 years receive cervical cancer screening [3], due to competing health needs, poor healthcare services, lack of financial resources, lack of trained health care professionals, lack of screening tests and lack of awareness among women [4].
Single visit approach (see and treat) using VIA has proven effective cervical cancer screening method in resource poor settings such as Ethiopia [5]. The World Health Organization (WHO) recommends HPV test followed by VIA if there are resources to provide HPV tests and sequence of tests; HPV alone if not able to provide sequence of tests; or VIA alone if HPV test is not available. Cervical cancer screening is recommended for women ages 30 to 49 years at least once in a lifetime and women younger than 30 years only if HIV positive or live in high HIV prevalence area [6]. The WHO also recommends targeted HPV vaccination of girl’s ages 9 to13 years [7].
There is no national cervical cancer-screening program, HPV DNA testing capability or HPV vaccination in Ethiopia. VIA is only available through pilot or demonstration programs. The ministry of health recently announced that 81 doctors and nurses have been trained to provide cervical cancer screening in 25 hospitals in five regions of the country [8]. However, it is not clear whether implementation is in effect.
The purpose of this study was to develop a curriculum on cervical cancer screening for medical students in years four to six at SPHMMC in Ethiopia and to assess improvement in knowledge and clinical skills based on the implementation of the curriculum.
Methods
Study Setting
This study was conducted at SPHMMC in Addis Ababa, a capital of Ethiopia, a country with estimated 102 million people [9]. St Paul’s is a specialty hospital providing care to the underserved population of Addis Ababa and the neighboring Oromia region. St Paul’s launched its medical education program in 2007 [10]. This study protocol was reviewed and exempted by the University of Michigan and SPHMMC IRB.
Study Team
The study team consisted of the principal investigator (PI) responsible for the design and implementation of the study and Obstetrics and Gynecology faculty at SPHMMC who facilitated local IRB approval, scheduling, acquisition of space/materials and recruitment of participants.
Subjects
All medical students in years four, five and six doing Obstetrics and Gynecology rotation during the study period were invited verbally to participate in the study voluntarily. This was a convenience sampling. Medical students were selected as participants because cervical cancer screening education is not provided in medical schools in Ethiopia. Medical school in Ethiopia is combined with undergraduate lasting six years. The final year (M6) is considered an internship after which graduates become general practitioners without further training.
Study Design
Knowledge and clinical skills based cervical cancer screening training with pre- and post-training assessment was provided. The training consisted of didactics on cervical cancer epidemiology, pathophysiology, screening methods, diagnosis and treatment of precancerous lesions and a practicum. A power point presentation was used in teaching medical students. Speculum examination and VIA training were planned, but only speculum examination on a pelvic model was done due to logistical reasons. The majority of the participants had no prior speculum examination experience, their schedules did not allow for extended training and there was no process in place to recruit patients for speculum examinations.
The assessment was done using survey adopted from a previously validated survey by Levin et al. [11]. The survey consisted of Likert scale, multiple choice and open-ended questions. Questions about demographics information were added and some questions were removed from the original survey. The pre- and post-training surveys were similar except the post-training survey consisted of the open-ended questions.
Data Collection
Data was collected during two one-hour sessions consisting of 1) pre-training assessment and power point presentation, and 2) practicum on speculum examination and post-training assessment. The first session was in a classroom with chairs and tables arranged in rows facing the front where there was a whiteboard and a desk. Laptop computer and a projector were set up on the desk. The PI stood at the front center of the classroom facing the students, described the study and obtained verbal consent. The participants were assigned a study number, which they wrote on the survey before completing. After completing the pre-training survey, the participants received a 20-minute power point presentation on cervical cancer screening, followed by questions and answers.
During the second session, M4 and M5 participants practiced speculum examination on a pelvic model and completed the post- training survey. The classroom was arranged in a curve facing the front. Pelvic model and metal speculum were set up on a table in front of the class. Facing the participants, the PI demonstrated how to perform a speculum examination followed by participants taking turn practicing. M6 participants only completed the post- training survey and did not perform speculum examination since they have been doing this on patients during their internship. The groups were divided in this fashion for logistical reasons and not to interfere with clinical duty.
Data Analysis
Knowledge of cervical cancer screening and comfort level on identifying cervical changes were assessed. The knowledge quiz consisted of 13 questions (twelve 1-point and one 2-points). For two questions that had “check all that applies” structure, a proportional credit was given for every correct answer selected and every incorrect one not selected. A question about cervical cancer methods of testing was a 1-point question comprised of 5 responses with a partial credit of 0.2 per question. Knowledge of cervical cancer risk factors was assessed using a 2-point question comprised of 8 responses with a partial credit of 0.25 per question. The final scores were expressed as percentages of a maximum absolute score of 13. Comfort level in identifying cervical changes was assessed using a 5-point Likert scale (1-not comfortable; 2-somewhat uncomfortable; 3-somewhat comfortable; 4- comfortable; 5-very comfortable).
Statistical Methods
McNemar’s binomial test, Wilcoxon signed rank test or Independent sample Kruskal-Wallis test were used as appropriate. Data was analyzed using SPSS 22 software (Chicago, IL).
Results
There were a total of 28 participants, 7 (25%) females and 21 (75%) males. When broken down by medical school year, 12 (43%) were M4, 6 (21%) were M5 and 10 (36%) were M6 participants. Twenty-three (82%) participants completed both pre- and post- training surveys, including all 12 M4, 5 out of 6 M5 and 6 out of 10 M6 participants.
Knowledge Assessment
Knowledge of cervical cancer screening significantly increased after the training. Based on 13 knowledge questions, a median pre- training total knowledge score was 55.9% (range 24.6 – 88.2%), while a median post-training score was 75 % (range 37.9 – 96.4%) (Wilcoxon signed rank test p=0.001).
A median baseline score for M4 participants was 57.6% (range 33.9-88.2%) and significantly increased to 75.2% (range 48.2- 91.1%) post-training (Wilcoxon signed rank test p<0.01) (Figure 1). A median baseline score for M5 participants was 53.6% (range 39.6-66.4%) and increased to 80.7% (range 45.0-96.4%) post- training (Wilcoxon signed rank test p=0.08) (Figure 1). A median baseline score for M6 participants was 56.6% (range 24.6-78.6%); an increase in the score was not statistically significant post- training (median 60.7%, range 37.9 – 85.7%) (Figure 1).
At baseline, more than 50% of the participants correctly answered the questions on cervical cancer prevention, an anatomical location of cervical cancer, most methods of testing and the majority of risk factors for cervical cancer. The lowest pre-training scores were on the lowest stage of cervical cancer detected by VIA, and the prevalence and mortality of cervical cancer in Ethiopia (Table 1). Most of the scores increased after the training. Particularly, significant increase was observed for the questions about 1) concentration of acetic acid used for VIA (from 34.8% to 69.6%, McNemar’s binomial test p<0.01), 2) the role of vaccination in the prevention of cervical cancer (from 73.9% to 100%, p<0.05), 3) an anatomical location of cervical cancer origin (from 52.2% to 78.3%, p<0.05), and 4) the prevalence of cervical cancer among women in Ethiopia (from 17.4% to 52.2%, p<0.05) (Table 1).
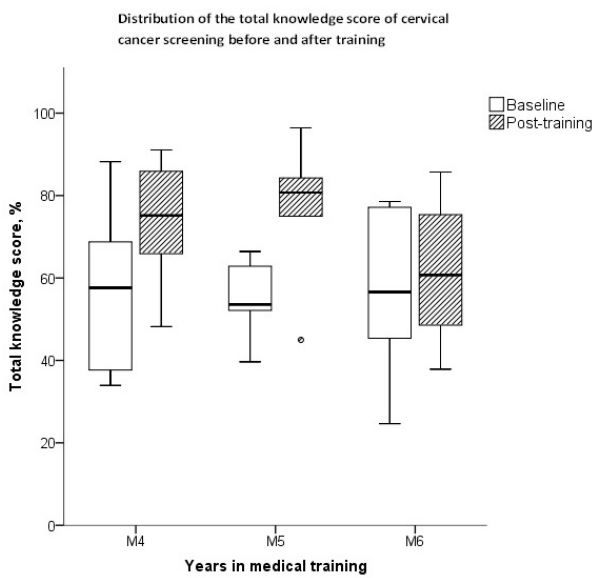
Figure 1: Distribution of the total scores for knowledge about cervical cancer screening before and after the educational intervention by the year of medical training. Data are presented as box plots with horizontal lines on the bars defining group medians. The data for the participants who completed both pre- and post-training surveys are shown (N=23), including 12 M4, 5 M5 and 6 M6 participants.
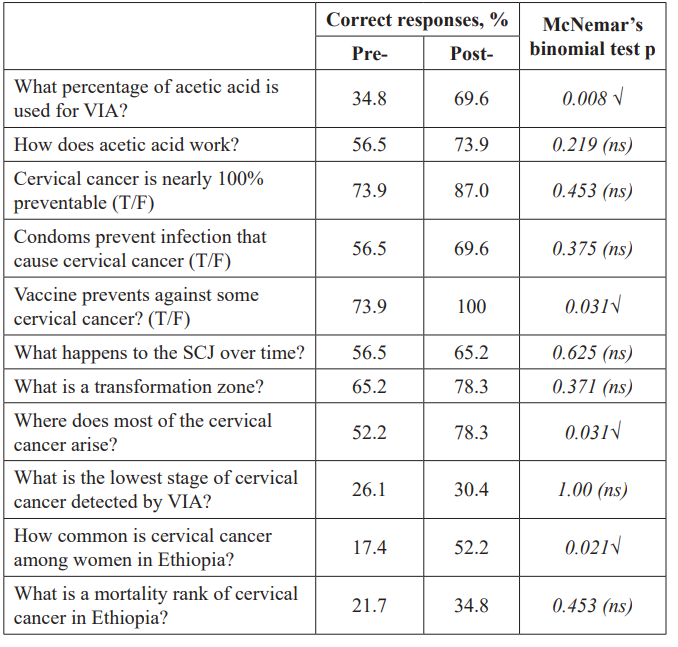
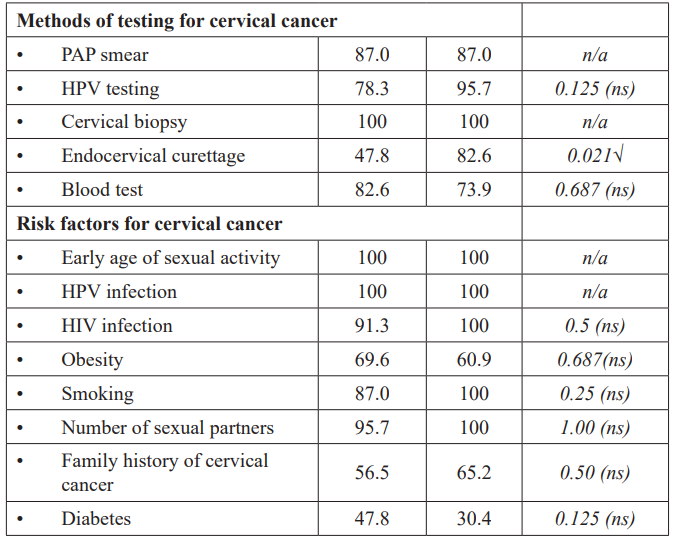
Table 1: Responses to individual knowledge questions about cervical cancer before and after the educational intervention, (N=28), Ethiopia, 2013.
The data for the participants who completed both pre- and post-training surveys are shown (N=23).
VIA: Visual inspection with acetic acid; T/F: True/False; SCJ: Squamocolumnar junction; √ : Significant at α=0.05; ns: Not significant; n/a: Not applicable (no change).
At the baseline, only 3 out of 23 participants (13%) demonstrated knowledge of cervical cancer risk factors, and the results were unchanged after the training. There was an inconsistency in the responses about the association of obesity and diabetes with cervical cancer. Some participants responded correctly before the training and incorrectly after the training resulting in a smaller proportion of correct answers after the training compared to the baseline, although the differences were not statistically significant (Table 1).
Clinical Skills Assessment
A baseline, speculum examination experience varied by year in medical school and increased with an advanced medical school year from a median of 0 cases (range 0-2) for M4, a median of 0 cases (range 0-3) for M5 and a median of 3 cases (range 0 -10+) for M6 participants (independent sample Kruskal-Wallis test p<0.01, N=27). M4 and M5 participants reported higher number of speculum examinations post-training compared to baseline although the differences were not statistically significant (Figure 2).
Only 1 participant (4%) was trained in VIA before the training. Before the training, 75% participants were familiar with the term “aceto-white epithelium” and its significance. These proportions increased to 95.5% post-training, although the differences were only marginally statistically significant (McNemar’s binomial test p ≤ 0.1).
A median score for the level of comfort in identifying aceto-white changes was 2 (range 1-5) pre- training, and increased to 3 (range 1-5) post-training, however, the difference was only marginally significant (Wilcoxon signed rank test p<0.1). Prior to the training, 52% reported some level of comfort in identifying aceto-white changes (score 1) versus 82% post-training (McNemar’s binomial test p<0.05).
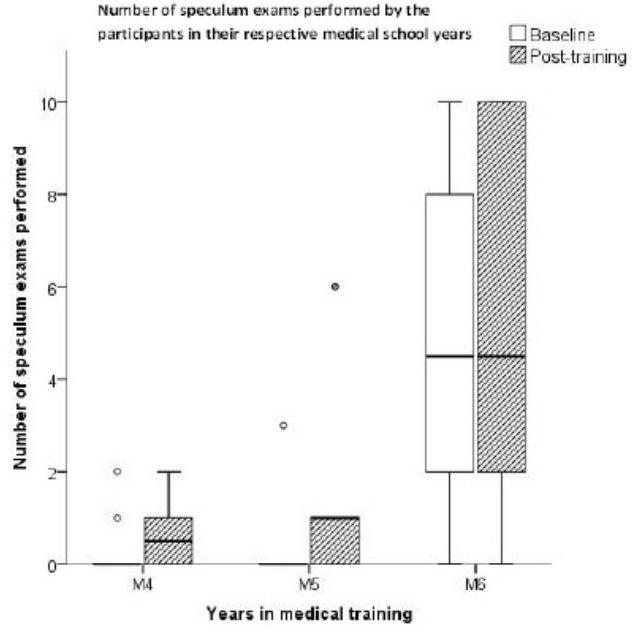
Figure 2: Number of speculum exams performed by the participants in their respective medical school years. Data are presented as box plots with horizontal lines on the bars defining group medians. The data for the participants who completed both pre- and post-training surveys are shown (N=23), including 12 M4, 5 M5 and 6 M6 participants.
A median level of comfort in identifying mosaicism and punctation was 1 (range 1-5) prior to the training, and increased to 2 (range 1-5) post-training, although the difference was only marginally statistically significant (Wilcoxon signed rank test p<0.1). The proportion of participants with some level of comfort increased from 48% pre-training to 70% post-training, however the difference was not statistically significant.
Discussion
The participants were mostly males reflecting the gender distribution in higher education institutions in Ethiopia. Medical education in Ethiopia consists of undergraduate and postgraduate programs. The undergraduate programs award Medical Doctor degree while postgraduate programs award specialty certificates. In the academic year 2014-2015, of those enrolled in an undergraduate Medicine and Health Sciences program, 34.7% were females at government institutions and 58.6% at non- government institutions. For post-graduate Medicine and Health Sciences programs, 37.5% in government institutions and 36.4% in non-government institutions were females. Out of total 27, 640 academic staff at both government and non-government higher education institutions, only 3,070 were women [12].
The response rate was overall very good except for M6 participants, which was lower than both M4 and M5 participants. M6 participants were doing their internship and likely had clinical responsibilities that took precedence. The majority of medical students become general practitioners upon graduation from medical school and could be in a position to provide cervical cancer screening if they receive adequate training. Providing cervical cancer screening training at post-graduate level is limited due to limited number of post-graduate training programs and few numbers of residents in those programs. Additionally, those completing postgraduate programs practice specialty care and are less likely to engage in screening programs. As such, it is important to provide basic knowledge and clinical skills of cervical cancer screening at the undergraduate medical education level.
In our study, the total knowledge scores improved significantly (55.9% pre-training and 75% post-training; p=0.001). The increase was statistically significant among M4 participants (M4 57.6% to 75.2%, p<0.01) although there was an improvement in scores in all three years. This maybe because M6 participants were more focused on their clinical responsibilities and less engaged in the training. The baseline scores for all participants were similar regardless of medical school year. Although the training in this study was short and there was no time for repetition, the outcome in knowledge enhancement was significant. This suggests that it is possible to improve cervical cancer screening knowledge through short educational training such as the one used in this study.
Knowledge about VIA was low since VIA is not taught in medical schools despite WHO’s recommendation to use VIA as cervical cancer screening tool of choice in resource poor areas [6]. Additionally, knowledge about methods of cervical cancer screening was low at baseline, but significantly improved after training (30.4% to 47.8%, p<0.05). This reflects the lack of training on cervical cancer screening and the low rates of screening in the country. Knowledge about prevalence, mortality rate and risk factors for cervical cancer was low although cervical cancer is the 2nd leading cause of cancer and the leading cause of cancer related deaths among women in Ethiopia [3]. The knowledge about prevalence of cervical cancer among women in Ethiopia increased from 17.4% to 52.2% (p<0.05). Only 13% of the participants knew risk factors for cervical cancer at baseline and this did not improve with the training. This highlights the need for increased awareness about cervical cancer among medical students. Moreover, there was inconsistency in reporting pre- and post-training indicating that the participants have superficial knowledge at baseline and need additional training to solidify their knowledge.
The training provided was more knowledge-based than skills-based leading to more significant increase in knowledge than clinical skills scores. Although the majority of participants reported being familiar with the term aceto-white epithelium and its significance at baseline, this improved only with marginal significance (75% to 95 %; p<0.1) after the training. Comfort level in identifying aceto- white changes, mosaicism and punctation were low at baseline (2 and 1 on 0 to 5 scale, respectively) and again increased with only marginal significant post-training (3 and 2, respectively; p<0.1). This is likely due to participants’ over-reporting about their familiarity with aceto-white changes at baseline. The low comfort level at baseline indicates need for further training.
The results for speculum examination were as expected with median of zero cases for M4 and M5 participants and median of three cases for M6 participants. Students learn how to perform speculum examination during their internship year (M6). Although the participants used pelvic model for speculum examination in this study, the M4 and M5 participants reported higher number of speculum examination post-training. It is unclear if they performed additional speculum examinations outside of the training although this is less likely. This was most likely over reporting. Speculum examination is the most basic clinical skill for cervical cancer screening. This very basic and essential skill should be taught early in medical school to provide opportunity for repetition and to develop competency on speculum examination before provision of clinical care.
In addition to the numbers showing the need for cervical cancer screening training among medical students, the students themselves voiced interest in obtaining more training. During the study, M4 and M5 participants engaged more in the training than the M6 participants. Although very few students seek out opportunity for training, they showed desire for more hands on cervical cancer screening experience. They are more likely to participant in cervical cancer screening training if offered rather than seeking this opportunity out.
Limitations
Sample size was small and all participants were from one medical school, which may limit generalizability of the findings. Limited communication beforehand, logistical issues and limited knowledge of the setting and the system at SPHMMC prevented incorporation of speculum examination and VIA on live patients as was originally planned. The training provided significantly improved the overall knowledge about cervical cancer, however, did not achieve similar outcomes in clinical skills improvement. Future studies should incorporate both knowledge and clinical skills based training and to include participation of other medical schools, residents as well as other health care providers (e.g. Nurses and Nurse Midwives). Knowledge retention should also be assessed with future studies.
Conclusions
The findings in this study show there is significant gap in knowledge and lack of basic clinical skills of cervical cancer screening among Ethiopian medical students at SPHMMC. This study demonstrated that it is possible to improve knowledge and clinical skills of cervical cancer screening with short training with limited resources. Future efforts should focus on incorporating didactics and clinical skills based training on cervical cancer screening into medical schools, postgraduate training programs and other health professional programs. Effective cervical cancer prevention in Ethiopia requires increased awareness and improved training.
Acknowledgements
This work was made possible through the generous support of St Paul’s Hospital Millennium Medical College and the University Of Michigan Department Of Family Medicine. We thank Dr. Michael Fetters, Dr. Katherine Gold and Dr. Senait Fisseha for their contribution to this study.
References
- Globocan 2012: Estimated Cancer Incidence, Mortality, and Prevalence Worldwide in
- Gakidou E, Nordhagen S, Obermeyer Coverage of cervical cancer screening in 57 countries: low average levels and large inequalities. PLoS Med. 2008; 5: e132.
- http://www.hpvcentre.net/statistics/reports/ETH_FS.pdf
- Denny L, Quinn M, Sankaranarayanan Screening for Cervical Cancer in Developing Countries. Vaccine. 2006; 24S3:71-77.
- Goldie SJ, Gaffikin L, Goldhaber-Fiebert JD, et al. Cost- effectiveness of cervical-cancer screening in five developing N Engl J Med. 2005; 353: 2158-2168.
- http://apps.who.int/iris/bitstream/10665/94830/1/9789241548694_eng.pdf?ua=1
- http://www.who.int/immunization/hpv/learn/comprehensive_pdf
- http://www.moh.gov.et/documents/26765/1612928/Annual+ Performance+Report+EFY2005/edac28ed-1365-4d9a-b734- ac4fc352de5e?version=1.1
- https://www.cia.gov/library/publications/the-world-factbook/geos/et.html
- http://globalreach.med.umich.edu/sites/default/files/files/Porter,%20Annie_Ethiopia.pdf
- Levine LD, Chudnoff SG, Taylor K, et al. A 5-day educational program for teaching cervical cancer screening using visual inspection with acetic acid in low-resource settings. Int J Gynaecol 2011; 115: 171-174.
- http://www.moe.gov.et/en_US/-/education-statistics-annual-abstract-2007-e-c?inheritRedirect=true