Ethno-Regional Variations in the Proportions and Frequencies of Dilatation And Curettage, Open Myomectomy and Caesarean Section
Author'(s): Abayomi Ajayi1, Bamgboye M. Afolabi2*, Victor Ajayi1, Ifeoluwa Oyetunji1, Oluwafunmilola Biobaku1, Happiness Aikhuele1, Arati Sohoni1, and Oluseun O. Saanu1
1Nordica Fertility Center, 106 Norman-Williams Street, Ikoyi Lagos, Nigeria
2Health, Environment and Development Foundation, 34 Montgomery Road, Yaba, Lagos
*Correspondence:
Bamgboye M. Afolabi, Health, Environment and Development Foundation, 34 Montgomery Road, Yaba, Lagos, Tel: +2348058658029; E-mail: bmafolabi@gmail.com.
Received: 08 June 2017 Accepted: 05 July 2017
Citation: Abayomi Ajayi, Bamgboye M. Afolabi, Victor Ajayi, et al. Ethno-Regional Variations in the Proportions and Frequencies of Dilatation And Curettage, Open Myomectomy and Caesarean Section among Women With and Without Intra-Uterine Adhesion a Sub-Saharan Setting. Gynecol Reprod Health. 2017; 1(2): 1-10.
Abstract
Background: Intrauterine adhesion (IUA) occurs when trauma to the endometrial lining triggers the normal wound-healing process, which causes the damaged areas to fuse together. Termination of pregnancies, miscarriages and other gynecological operations are likely risk factors for IUA.
Materials and Methods: This was a retrospective study of 902 Nigerian women who patronized Nordica Fertility Center for fertility evaluation. Hysteroscopy was used to assess uterine abnormalities. The information extracted from the patients’ medical records included age, body mass index, ethnic group, parity, performance, type and number of uterine surgeries. Ethnic grouping was cross-tabulated against other variables using STATA-13. Chisquare and t-test, were used to determine statistical differences in means and proportions and Linear regression analysis was used to ascertain correlations between variables. A P-value of <0.05 was considered significant.
Results: The mean (±sd) age (years) of the 902 surveyed was 38.7 (6.1) with no significant difference among women from Southwest and south-south (38.8 ± 6.2 respectively), Southeast (38.4 ± 5.9) and the North (37.4 ± 5.1). Majority (478, 52.8%) of the women were from the Southwest, the region that also produced the highest proportion of professional occupation (217, 45.4%). Overall mean (±sd) Body Mass Index was 27.8 (4.9) with women from the North slightly heavier (28.5 ± 4.4) than others. The highest proportion (85.2%) of nulliparous women were from the North. Majority (51.0%) of the women with IUA were from Southwest and only 3.0% were from the North of the country. Among women with IUA, those from the North had the highest mean number of Dilatation and Curettage (3.29 ± 1.60), those from the Southeast had the highest mean number of Open myomectomy (1.19 ± 0.47) and those from the Southwest the highest mean number of Caesarean section (1.50 ± 0.53) performed. Also, among women with IUA, the ratio of D&C per woman was highest in the North (2.9:1), while that of Open myomectomy per woman was highest in both Southeast (0.66:1) and South-south (0.66:1). The ratio of Caesarean section per woman was highest in South-south (0.34:1). The strongest positively significant correlation between performance of uterine surgery and ethnicity was found with Caesarean section (r=0.58, Std. Err.=0.014, t=39.74, P-value<0.00001, 95% CI: 0.56, 0.61). The strongest positively significant correlation between quantity of uterine surgery performed and ethnicity was found with Dilatation and Curettage (r=0.43, Std. Err.=0.022, t=19.65, P-value<0.00001, 95% CI: 0.39, 0.47).
Conclusion: Data from this study shows some significant ethno-regional differences in the performance and quantity of uterine surgeries/procedures in different regions of Nigeria. Frequent training of medical doctors and other health workers in correct diagnosis, application of modern gynecological instrumentation and proper management of patients could reduce unnecessary uterine interventions and the attendant morbidity of intrauterine adhesions.
Keywords
Introduction
Hardly does any evidence exist in literature concerning incidences of intrauterine adhesions among various ethnic groups in the world. Such evidence would be helpful to not only gynecologists and health care professionals but also to policy-makers when considering the burden of infertility and gynecological illnesses among women. One of the very few studies linking adhesions to women of different races was conducted in Canada by Tulandi et al., [1] in which they described postsurgical adhesions as comparable to keloid which do not regress spontaneously, tend to recur after excision and are rare in Caucasians than in African Americans.
In India, a country of diverse culture and ethnicity, there is, surprisingly, scanty data regarding Asherman’s syndrome and its type of presentation, severity of adhesions, recurrence and impact on menstrual pattern [2-4]. Disease presentation in Indian subcontinent is distinguished by different incidence of etiological factors and not ethnic variations. For example, it has been shown that genital tuberculosis is associated with recurrence of IUA and poor prognosis after hysteroscopic surgery, though no mention is made of the ethnic background of patients [5].
Nigeria, like India, is also a multi-culture, multi-lingual and multi- ethnic country located in West Africa with an estimated population of about 180 million. The major ethnic groups are the Yorubas in the Southwest, the Igbos in the Southeast and the Hausa-Fulanis, the Kanuris, Tivs and Idomas in the North. Since the demarcation of the country into six geo-political zones and a Federal Capital Territory, other ethnic groups became recognizable, playing vital and prominent roles in the polity of the nation. Such ethnic groups include the Nupes, Igalas, and Gbagyis in the North-central and the Izons, Binis. Ijaws, Efiks, Ibibios and others in the South-south geo-political zones.
In general, adhesions are fibrous strands/bands of tissue that result from wound-healing process and connect tissues or organs that are naturally separate [6]. Specifically, various invasive gynecological procedures are potentially responsible for the development of intrauterine adhesions and women on who tubal, ovarian or uterine procedures (such as treatment of endometriosis, and myomectomy) are performed, are at high risk. According to Dean and Abbott [7], the true incidence of IUA is unknown and difficult to establish “because the condition is rare in the general population and often asymptomatic,” quoting a range from 1.5% in incidental finding at hystero-salpingogram to 21.5% of those with a history of postpartum uterine curettage. Earlier studies in Nigeria [8,9] had shown that IUA occurs in approximately 20% of women consulting for infertility, though this figure may not reflect the true picture of the condition in the community. Al-Inany [10] gave an impression that globally, IUA affect women in different ages and that there is no fundamental genetic preference in its development.
It is important to diagnose intrauterine adhesions as they are often associated with menstrual abnormalities, miscarriage and infertility. Though no genetic pre-disposition has been associated with intrauterine adhesion and since the incidence of IUA in the general population of indigenous Black African is not known, the facility-based prevalence of IUA among a large sample size may give an idea of the geographical spread within a community or in a country. Also, the outcome may stimulate a further probe into regional or global prevalence of the condition. There is paucity of information on IUA in African population and furthermore, data are very scanty on ethnic variations in gynecological processes that lead to IUA among African population. This study focused on bridging the gap in information that exists on likely ethno- geographical variations in the gynecological procedures and the development of IUA among Nigerian women of different ethnic origins.
Materials and Method
The country, Nigeria, is located in West Africa, between Benin Republic to the west and Cameroon to the east and bordered to the south by the Gulf of Guinea of the Southern Atlantic Ocean and to the north by the Sahara dessert. Its current population is approximately 180 million, making it the most densely populated African nation and the largest black country globally. From its southern edge, its terrain fluctuates from the oil-rich Niger-Delta, through to a belt of rain forests inland, to the high savanna-covered plateaus and arid regions in the north. There are at least 400 diverse ethnic groups (with about 450 different languages) that make up the population of the country, the three largest being (i) the Hausa- Fulani (29% of the population) in the north (ii) the Yoruba (21%) in the Southwest and (iii) the Igbo (or Ibo) (18%) in the Southeast. The country is split into six major ethnic groups along the geo- political zones or regions, comprising the Hausa Fulani in the North West, Kanuri in the North East, Tiv in the North Central, Igbo in the South East, Yoruba in the South West and Ijaw in the South-south. The North East, North West, South-south and North- central regions of Nigeria are made up of diverse ethnic groups, while the South East and South West are predominantly Igbos and Yorubas respectively. The ethnic groups in each of these regions have their similar and dissimilar economic activities such as Cattle, Agriculture and Commerce in the Northeast, Northwest and North-central; Commerce, Farming, Fishing, Herbal Medicine, Industrialization, Tye and Dye, Textile and Banking and Finance in the Southwest; Coal, Commerce, Agriculture, Industrialization, Granite and Palm-wine in the Southeast; and Oil and Gas, Farming, River sand, Rubber, timber, Periwinkle shell and Nut shell in the South-south. These areas also yield diverse agricultural products and minerals. Patients in the study were thus classified according to volunteered ethnic group each claimed (Figure 1).

Figure 1: Ethno-regional map of Nigeria (Source: http://www.learnnc.org/lp/multimedia/8819 ).
Data from the study was derived from patients’ medical records in three cities – two from the southern part of Nigeria (Lagos and Asaba) and one from the north (Abuja) where Nordica Fertility Center provides gynecological and Assisted Reproductive Technology (ART) services. Patients reporting at any of these three cities for infertility-related health problems were evaluated as per facility protocol which included a comprehensive history, seminal fluid analysis (for male partners), baseline transvaginal ultrasound and routine blood investigations (including Follicle Stimulating Hormone (FSH), Luteinizing Hormone (LH) and Prolactin). Patients were included in the study if they fulfilled certain criteria such as (i) History of previous adnexal surgery (ii) Diagnosis of intrauterine adhesion with no other demonstrable cause(s) of infertility (iii) Recurrent miscarriages before presentation. Conditions for excluding patients from the study were (i) Presence of pelvic cancer (ii) Uterine malformation (iii) Consent not given to use data for studies.
In the period between June 2005 to November 2014, 3138 patients were seen at Lagos, Asaba and Abuja offices of Nordica Fertility Center in Nigeria. Hysteroscopy was performed for 1,115 (35.5%) of these patients but data of only 905 (81.2%) women who met the inclusion criteria were extracted, cleaned and analyzed. The remaining women had incomplete data such as missing age, weight or body mass index, ethnic group and type and/or frequency of uterine surgery performed and were excluded from the study.
Capacity building: Capacity of three data recording officers was enhanced for retrieving data from medical records of the study patients, coding, entering the data into a laptop and cleaning the data. These data recording officers were supported and administered by a seasoned obstetrician/gynecologist in the team (OB).
Local Ethics Committee approved the study. Hysteroscopy was performed to evaluate and treat the presence of intrauterine abnormalities. The operating surgeons gave detailed explanation of the procedure involved in hysteroscopy to each patient, and all women signed an informed consent before undergoing hysteroscopy. Part of the informed consent concerns the use of data for teaching, training and research purposes. Step-by step discoveries at hysteroscopy were manually documented on the case note of each patient.
The patients were put under short general anesthesia (GA) before the hysteroscopy procedures were performed. The instrument used was a rigid 20-degree 5-mm hysteroscope consisting of an operative channel for the manipulation of grasping forceps, scissors, or bipolar electrode. A diagnostic hysteroscopy was first done in all cases then relevant instruments were placed via the operative channels to carry out surgical treatment on any identified pathology if indicated and where endometrial biopsies were necessary they were taken. Other details of the materials and methods are available elsewhere [11].
Definitions and groupings
Age group was categorized by a five-year interval from 25 to 50 years. Ages below 25 and above 50 were not categorized by the 5-year interval. Body Mass Index group was categorized according to the WHO classification: <18.5=underweight; 18.5 to 24.99=normal, 25.0-29.99=overweight; ≥30=obese [12]. Marital status was stratified as single if there has never been a conjugal matrimony and ever married if there has ever been such matrimony.
Statistical Analysis
Analysis was done using STATA 13 and the level of significance was set at P<0.05. Descriptive statistics were presented as numbers and percentages for qualitative data, mean and standard deviations for quantitative data. Data was presented as tables and graphs.
Results
All the 3138 cases-notes of patients who consulted at Nordica Fertility Center between June 2005 and November 2014 were retrieved. A total of 1,115 (35.5%) of them had performed hysteroscopy for the examination of uterine cavity and among these the records of 905 women were extracted for analysis of interest, that is, the ethnic distribution of intrauterine adhesions and other related conditions. Among the Nigerian ethnic groups in the study, those from the Southwest formed the majority (478, 52.8%) of the patients, followed by women from Southeast (221, 24.2%) while women from North (27, 3.0%) were the least in number (Table 1). Means of age (years) and Body Mass Index (Kg/m2) indicate that women were not significantly different though women from North were slightly heavier (28.5 ± 4.4) than the rest. The highest proportions of professionals (217, 45.4%), Chief Executives (15, 6.8%), women in Banking and Finance (54.5%) and civil/public servants (22, 4.6%) were from Southwest, Southeast, South-south and Southwest respectively. The proportion of nulliparous women was highest (23/27, 85.2%) in the North and least among those from Southeast.
Age distribution of the women also varies according to their region, as illustrated in Figure 2. Generally, there were very few women below the age of 25 years from any region. However, the highest proportion of women aged 25-30 years (11.8%) was from Southeast; those aged 31-35 years (37.0%) and 36-40 years (33.3%) were from the North; (iii) those aged 41-45 years (28.4%) and 46-50 years (12.5%) respectively were from South-south while those aged >50 years (3.7%) were from the North.
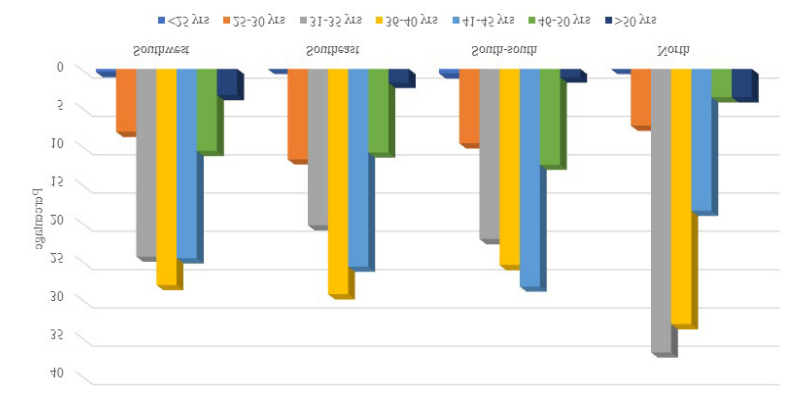
Figure 2: Distribution of age groups of patients from different geographical regions.
The overall facility-based prevalence of IUA was 29.2%, distributed as 51.0% among women from Southwest, 24.7% among those from South-east, 20.1% among women from the South-south, and 3.0% among women from the North (Table 2). Though there were no significant differences in the proportions of women with and without IUA, women from South-south region (OR=1.17, 95% CI: 0.82, 1.67) were observed to be approximately 1.2 times more likely to have IUA compared to women from other regions.
The mean number of reported D&C, OM and CS performed on all women was calculated (Table 3). Overall, the mean number of D&C performed among IUA-positive women (2.48 ± 1.71) was significantly higher (t=2.52, P-value=0.006) than that performed among the IUA-negative women (2.10 ± 1.46). This significant difference appears to have been driven by the mean number of D&C performed mainly among women from Southwest (t=2.02, P-value=0.02). Regardless of whether IUA-positive or IUA- negative, there was no significant difference in the mean number of D&C performed when each ethnic group was compared with others.
Of the 263 IUA positive women, 179 (68.1%) had performed a minimum of one D&C and a maximum of nine. Among the 639 women without IUA, 337 (52.7%) had performed a minimum of one D&C and a maximum of 10. The largest proportion of women with IUA who had performed D&C was from Southwest (86/179, 48.0%) and the least was from the North (7/179, 3.9%). The highest mean number of D&C performed (3.29 ± 1.60) occurred among women from the North and the least (2.29 ± 1.61) among women from Southeast.
Of the 130 women with IUA who had undergone OM, 59 (45.4%) were from Southeast and only 3 (2.3%) were from the North. Among the 192 women who were IUA negative, the highest proportion of 109 (56.8%) were from Southwest and the lowest, 6 (3.1%), were from the North. The highest mean number of OM performed (1.19 ± 0.47) occurred among women from Southeast while the highest mean number of OM (1.18 ± 0.45) performed on women without IUA occurred in South-south. Overall, there was no significant difference (t=0.64, P-value=0.26) in the mean number of open myomectomy performed among IUA-positive (1.17 ± 0.43) and IUA-negative (1.14 ± 0.39) women and among the various ethnic groups from the regions.
A substantial alteration was observed (t=1.65. P-value=0.05) in the overall mean number of Caesarean section performed among those who were IUA-positive (1.35 ± 0.49) compared with those who were IUA-negative (1.65 ± 0.05). This significant difference seems to have been driven by the mean number of Caesarean sections performed mainly among women from Southwest (t=2.06, P-value=0.03). although Southeast region had the highest proportion (42.3%) of women with IUA who had Caesarean section performed on them as against 3.8% and 15.4% of women from the North and the South-south regions respectively.
As illustrated in Figure 3, D&C was the predominant uterine surgical procedure of all uterine interventions in all the regions. D&C was more prevalent among women with IUA than among those without IUA. Open myomectomy was less common but it was more prevalent among those with IUA than among those without IUA.
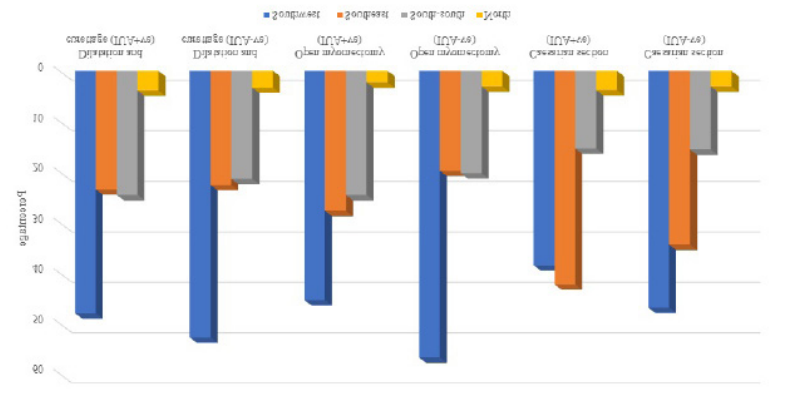
Figure 3: Proportion of women from various regions by type of uterine surgery/procedure relative to presence or absence of IUA.
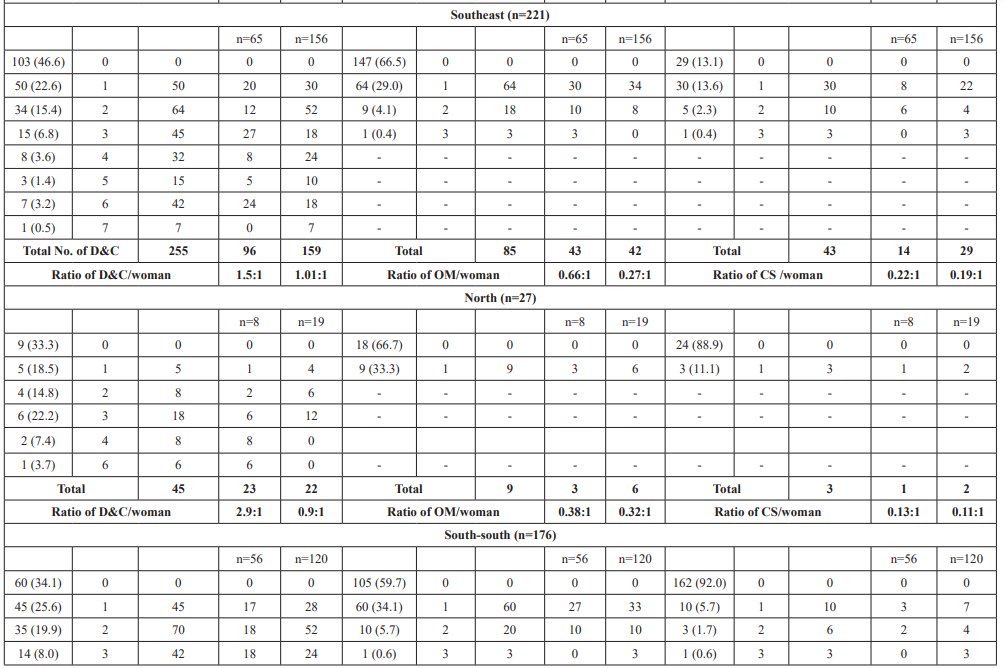
The ratios of D&C, Open myomectomy and Caesarean section per woman with IUA varied in each region and among the various ethnic groups (Table 4). For example, among women from the North, the ratio of D&C per woman was (2.9:1); 2.04:1 among women from South-south; 1.6:1 among women from the Southwest and 1.5:1 among those from Southeast zone. On the other hand, the ratio of Open myomectomy per woman was 0.66:1 among women from Southeast and South-south respectively, and only 0.38:1 among women from the North. The ratio of Caesarean section per woman was 0.34:1 among women from South-south and only 0.11:1 among those from Southwest. The Table also illustrates that D&C was the commonest uterine procedure performed among women in all regions.



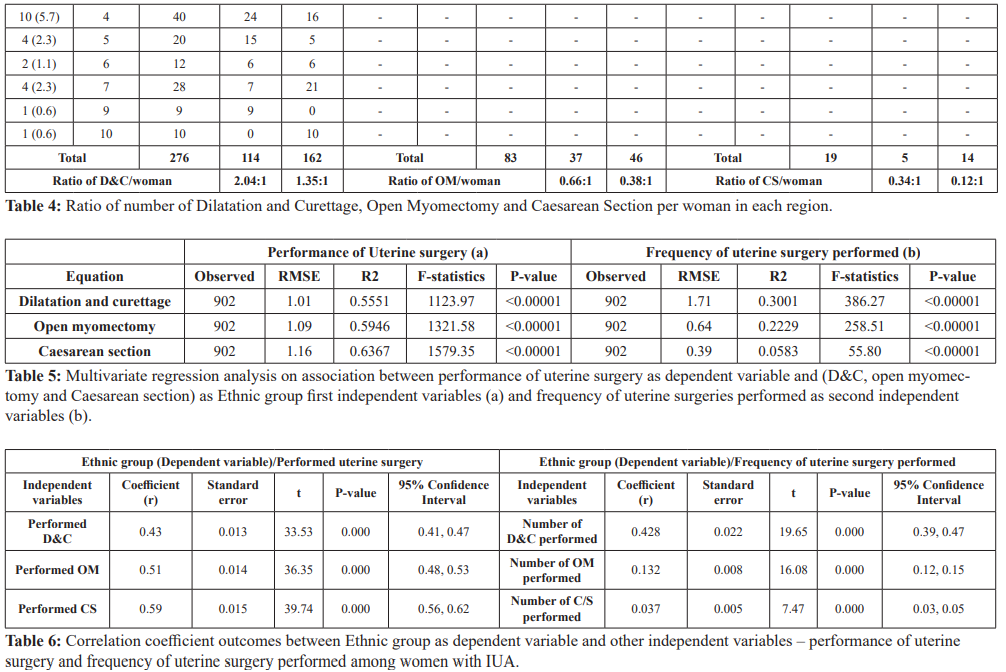
Multivariate regression analyses showed a significant correlation between ethnicity (independent variable) and whether a woman performed uterine surgery or not (dependent variable) (Table 5). Caesarean section accounted for the highest (63.67%) fragment of the explanation for variations in performance of uterine surgery (r2=0.6367, F=1579.35, P-value<0.00001) while D&C accounted for the highest (30.01%) portion of clarification for the quantity of uterine procedure/surgical interventions performed (r2=0.3001, F=386.27, P-value<0.00001). As shown in Table 6, the strongest positively significant correlation between performance of uterine surgery (dependent variable) and ethnicity (independent variable) was found with Caesarean section (r=0.58, Std. Err.=0.014, t=39.74, P-value<0.00001, 95% CI: 0.56, 0.61) and the strongest positively significant correlation between quantity of uterine procedure/surgical interventions performed (dependent variable) and ethnicity (independent variable) was found with Dilatation and Curettage (r=0.43, Std. Err.=0.022, t=19.65, P-value<0.00001, 95% CI: 0.39, 0.47).
Discussion
Very few studies have scrutinized the relationship between ethnic groupings and intrauterine adhesions after performances of uterine procedure/surgical interventions such as dilatation and curettage (D&C), open myomectomy (OM) and Caesarean section (CS). Consequent upon the large number of uterine surgeries reported (some evidenced during physical examination by abdominal scars) among women of varying ethnic backgrounds who patronized our facility for infertility-related problems, it was possible to evaluate intrauterine adhesions among these patients. This study was part of a larger retrospective study that investigated various aspects of intrauterine adhesions such as risk factors among Black African populations, menstrual abnormalities among women with IUA and occupational background of such women. For this study, analysis was limited to only indigenous Nigerians, though there were Europeans, Americans and other African nationals among the patients. The findings of intrauterine adhesions allowed us to examine more closely the association between Asherman’s syndrome, ethnic variations and mean and absolute number of procedures among women with and without IUA.
There are no studies in the literature that describe inter-ethnic prevalence of IUA among women of the same geographical origin anywhere. Part of the problem, especially in sub-Saharan Africa, lies in that most women with infertility often consult non-specialists and even when referred to a specialist, the cost of investigations such as hysteroscopy may be prohibitive. Another problem is that most gynecologists focus mainly on the presenting complain and may be eager to solve the problem without detailing the patient’s background. Of the 902 subjects included in this study, the majority 478 (52.8%) were from the Southwest while those from North accounted for only 1%. No rates of IUA for various ethnic groups, especially in Nigeria or in Africa, are available in the literature. This study may therefore be the first to document prevalence of IUA among various ethnic groups in sub-Saharan Africa.
There are certain key findings in this study. First, nulliparity was highest in the North (85.2%) followed by the Southwest (79.7%). This is a surprise finding because high fertility rate has been documented in Nigeria and Southwest has been known to have the highest twinning rate in the world [13]. For example, the frequency of twin births of 46.5 per 1000 deliveries and 46.2 per 1000 deliveries was recorded for towns such as Ilesa and Ile-Ife respectively, the centers of Yoruba land [14]. Several factors, such as (i) high level of infant and child mortality, (ii) early and universal marriage, (iii) early child bearing as well as child bearing within much of the reproductive life span, (iv) low use of contraception and (v) high social values placed on child bearing, are known to contribute to sustained relatively high levels of fertility in Nigeria [15]. The National Fertility Study (NFS, 1981/82) and the National Demographic and Health Studies (NDHS, 1990 and 1999) demonstrated high fertility rates in the country though these rates, by 1999, have decreased sharply in Southeast (6.8 in NDHS 1990; 4.6 in NDHS 1999) and Southwest (6.5 in NDHS 1990; 4.5 in NDHS 1999), but generally remained almost static in the North [15]. The 2013 NDHS puts this rate at 5.5 though it did not segregate it by regional difference [16]. Studies have however shown that nulliparity may be associated with increased risks for certain reproductive malignancies, including breast, ovarian and uterine cancers [17,18]. Nulliparity among the modern-day Southwest Nigerian women may be connected to their occupational dispensation as they are known to engage more in professional career, studentship, and Banking and Finance Industry and thus delay having children. Why nulliparity was observed to be very high among women from the North is not clear but may be related to increase in educational level of women and women making a stand against early marriage. Furthermore, it is very likely that, apart from increasing occupational and educational status, Northern parents are now eager to see that their girl-child is economically independent and does not succumb to societal vagaries and common illnesses that claim the lives of many children and young girls. Nulliparity has been associated with history of chronic hypertension, cigarette smoking during pregnancy, pre-pregnancy BMI and gestational diabetes mellitus in Latin American and Caribbean women [19].
Another major finding was that IUA was most prevalent (51.0%) in the Southwest which is higher than the 37.6% reported from Brazil [20]. The high prevalence of IUA in Southwest Nigeria may be related to the number and frequencies of D&C and other uterine surgeries conducted in the region. Also, probably because of relatively acceptable quality of health care in Southwest, many women may have gravitated to this region for uterine surgeries and high standard of quality of care. The reported incidence (new cases) of IUA in certain Nigeria cities were: 1.73% in Abuja [21]; 3.2% of all gynecological operations in Calabar [22] and 1.3% of new gynecological patients at Ilorin [23], though our study reported prevalence. It is expected that these prevalence of IUA may be lower than what is reported in this paper because our facility is specifically fertility-management oriented. While facilities in Abuja may attend to some women from North, those in Ilorin and Calabar would probably attend to women from North-central and South-south regions respectively.
In a 10-year Review of the Clinical Presentation and Treatment Outcome of Asherman's Syndrome at University of Maiduguri Teaching Hospital (UMTH) in Northeast Nigeria, Takai et al. [24] reported 8.1% (81/996) incidence of IUA among all gynecological operations.
It was surprising to observe that the North presented with the highest mean number of D&C (3.29 ± 1.60) and the highest ratio (2.9:1) of D&C per woman, compared to all other regions. It can only be speculated that early marriage and high rate of divorce could still be responsible for this high prevalence of D&C in this ethnic group and that high rate of D&C takes place at younger age group or after termination of pregnancy or consequent upon retained product of conception.
The mean number of Open Myomectomy was highest in the South- east region of the country (1.19 ± 0.47) indicating that fibroids may be more common in this region than in others. In all regions, the ratio of Open Myomectomy performed per woman was higher among women with IUA than among those without IUA. This may reflect the opinion of Conforti et al. [25] that “the risk of adhesions increased with increasing number of fibroids removed.” It is also possible that the risk of IUA probably increases with increase in the ratio of procedure per woman. Our data shows that, though the proportion of women without IUA (639, 70.8%) far outstrips that of those with IUA (263, 29.2%), the mean numbers of D&C and CS were significantly higher among those with IUA compared to those without IUA. This key finding illustrates that the quantity of D&C and CS performed may be significant risk factors than whether a woman had performed any of these uterine surgical interventions. An earlier study conducted in Southeast Nigeria found that, previous myomectomies, in which the uterine cavity was breached, was associated with 14% of intrauterine adhesions, which was lower than what is reported in our study [26]. The high rate of Open myomectomy among women from the Southeast of the country may be associated with aggressive gynecological surgeries by accredited and sometimes not-accredited health workers in this region.
Why fibroid may be more common in South-east Nigeria compared with the North is unclear, though this observed phenomenon may be related to the diet of the Northern women, which is mainly diary, millet and sorghum while consumption of red meat and leafy vegetable is widespread in the Southeast Nigeria. Further assessment is needed to verify this observation.
Another key finding was that the highest proportion of women who performed CS were observed to be from the Southeast, approximately twice the proportion of those from Southwest and South-south regions. This may be attributable to (i) gestational diabetes which leads to having big babies that may not easily pass through the birth canal and (ii) aggressive CS for most pregnancies, when CS is not needed. Caesarean section appears to be rare in the North compared to Southern region of the country. This may be attributable to strong aversion for Caesarean section due to belief that it reduces womanhood. It is possible that this is a critical factor that increases the rate of Vesico-vagina fistula (VVF), Recto-vagina fistula (RVF) and combination of VVF and RVF in the North.
Nevertheless, the exact reason for intrauterine adhesion growth has not been fully elucidated [26-29]. Non-surgical uterine procedures such as uterine fibroid embolization (UFE) have been noted to trigger intrauterine adhesions as reported in a study [25]. It is therefore very likely that several other factors – apart from age, previous history of uterine or abdominal surgery, and concomitant procedures that impede blood flow to the tissue – may play vital role in the development of IUA. Such factors may include blood group, concentration of certain minerals such as magnesium, calcium and zinc, in the body, or even immunoglobulins and other underlying systemic illnesses. Some authors have suggested a possible involvement of adhesion-related cytokines, such as b-fibroblast growth factor, platelet derived growth factor and transforming growth factor type 1, in the pathogenesis of IUA [30]. Others believe that vascular endothelial growth factor (VEGF) and increased micro-vessel density in patients responding to treatment, confirm that angiogenesis and revascularization may play an important role in endometrial regeneration [31]. In the final analysis, a genetic factor may clearly explain the reason behind certain patients’ pre-disposition towards adhesions incidence and recurrence [10,32,33].
Ultimately, hysteroscopy was used for final diagnosis and treatment while hysteroscopic lysis of identified adhesions [34] followed by the administration of broad-spectrum antibiotic concluded the management of all patients. It is advisable to conduct more studies in different parts of Nigeria and in other African settings to compare data with the findings in this study.
Conclusion
Analysis of 902 nulliparous and multiparous patients in Nigeria has provided new insight into the occurrence and frequencies of different uterine interventions and the incidence of intrauterine adhesions among women from different regions of Nigeria. The overall prevalence of IUA was 29.2% driven mainly by women from Southwest Nigeria. The Northern region supplied the highest proportion of nulliparous women. There was a significant difference (t=2.52, P-value=0.006; t=1.65, P-value=0.05) in the overall mean number of D&C and CS performed among women with IUA and those without IUA respectively. The ratio of D&C performed per woman was highest (2.9:1) in the North while the ratio of Open myomectomy performed per woman was highest (0.66:1) in both Southeast and South-south regions and that of CS (0.34:1) was highest in the South-south. The strongest positively significant correlation between quantity of uterine surgery performed (dependent variable) and ethnicity (independent variable) was found with Dilatation and Curettage (r=0.43, Std. Err.=0.022, t=19.65, P-value<0.00001, 95% CI: 0.39, 0.47).
Study limitations
This study has some limitations. First this was a facility-based survey and it may be inappropriate to make a sweeping statement of findings to the general population. Records are not properly kept and archived in most health facilities, otherwise it would have been easier to map the incidence of IUA by geographical locations in Nigeria. An additional reason why generalization may not be appropriate is that complete data was retrospectively reviewed for only 902 women compared to a women population of approximately 100 million. Secondly the data were from women who consulted at only three cities – Lagos, Asaba and Abuja which may have introduced residence bias since rural dwellers were not considered. Most clients were well-to-do who could afford the services for fertility treatment and were most likely in the middle to upper wealth quintile. This probably introduced inequity in data gathering. In general, there were very few women from the Northern Nigeria who consulted for infertility. Therefore, the paucity of data generated from Northeast and Northwest of the country did not do justice to ethno-geographical comparability of data. Be that as it may, another study is being planned to address this issue. Lastly, we did not investigate for infectious causes of IUA such as tuberculosis nor analyze the proportion of nulliparous women with or without IUA. These are left for further studies.
The strength of the study was predicated on the fact that the data on IUA was generated by specialists with long years of service and use of modern equipment. These specialists recorded their findings in patients’ medical records immediately the procedure was concluded. Patients’ medical records were kept safe and secure in hard copy. Data quality control was implemented for accuracy
References
- Tulandi T, Al-Sannan B, Akbar G, et al. Prospective study of intraabdominal adhesions among women of different races with or without Am J Obstet Gynecol. 2011; 204: 132.
- Roy KK, Baruah J, Sharma JB, et al. Reproductive outcome following hysteroscopic adhesiolysis in patients with infertility due to Asherman’s Arch Gynecol Obstet. 2010; 281: 355-361.
- Sharma JB, Roy KK, Pushparaj M, et Genital tuberculosis: an important cause of Asherman’s syndrome in India. Arch Gynecol Obstet. 2008; 277: 37-41.
- Malhotra N, Bahadur A, Kalaivani M, et Changes in endometrial receptivity in women with Asherman’s syndrome undergoing hysteroscopic adhesiolysis. Arch Gynecol Obstet. 2012; 286: 525-530
- Bukulmez O, Yarali H, Gurgan T. Total corporal synechiae due to tuberculosis carry a very poor prognosis following hysteroscopic synechialysis. Hum Reprod. 1999; 14: 1960-
- Wallwiener M, Brölmann H, Koninckx PH, et al. The Anti- adhesions in Gynecology Expert Panel (ANGEL). Adhesions after abdominal, pelvic and intra-uterine surgery and their Gynecol Surg. 2012; 9: 465-466.
- Deans R, Abbott Review of intrauterine adhesions. J Minim Invasive Gynecol. 2010; 17: 555.
- Giwa-Osagie OF, Emuveyan EE. Evaluation of secondary Nig Mad Pract. 1968; 7: 79-83.
- Otubu JA, Olarenwaju Hysteroscopy in infertile Nigerian women. Afr J Med Med Sci. 1989; 18: 117-120.
- Al-Inany H. Intrauterine adhesions: an update. Acta Obstet Gynecol 2001; 11: 986-993.
- Ajayi A, Biobaku O, Ajayi V, et al. Detection of Intrauterine Lesions by Hysteroscopy among Women with Fertility Challenges in an In-Vitro Fertilization Center in Lagos, Critical Care Obstetrics and Gynecology. 2015; 1: 8.
- http://apps.who.int/bmi/index.jsp?introPage=intro_3.html
- Smits J, Monden C. Twinning across the Developing World. PLoS 2011; 6: e25239.
- Akinboro A, Azeez MA, Bakare AA. Frequency of twinning in Southwest Indian J Hum Genet. 2008; 14: 41-47.
- Bamikale Feyisetan BJ, Bankole A. Fertility transition in Nigeria: Trends and Prospect. International Journal of Humanities and Social Science. 2014; 4: 506-528.
- National Population Commission [Nigeria]. Nigeria Demographic and Health Survey 1999. Calverton, Maryland: National Population Commission and ORC/Macro.
- Gleicher, Why are reproductive cancers more common in nulliparous women? Reproductive Biomedicine Online. 2013; 26: 416-419.
- Consorti, F, Tanna GD, Milazzo F, et Nulliparity enhances the risk of second primary malignancy of the breast in a cohort of women treated for thyroid cancer. World Journal of Surgical Oncology. 2011; 9: 88
- Conde-Agudelo A, Belizan Risk factors for pre-eclampsia in a large cohort of Latin American and Caribbean women. BJOG. 2000; 107: 75-83
- Salzani A, Yela DA, Gabiatti JRE, et al. Prevalence of uterine synechia after abortion evacuation Sao Paulo Med 2007; 125: 261-264.
- Efetie ER, Umezulike AC, Okafor Clinical and Demographic Characteristics of Women with Intrauterine Adhesion in Abuja, Nigeria. Obstetrics and Gynecology International. 2012; 4.
- Njoku C, Emechebe C, Eyong E, et Risk factors and management outcome of intrauterine adhesion in a constrained socio-economic environment: a 10-year review in the University of Calabar Teaching Hospital, Calabar. European Journal of Pharmaceutical and Medical Research. 2017; 4: 25-30.
- Abiodun OM, Balogun OR, Fawole AA. Aetiology, Clinical Features and Treatment Outcome of Intrauterine Adhesions in Ilorin, Central Nigeria. West African Journal of Medicine. 2007; 26: 298-301.
- Takai IU, Kwayabura AS, Ugwa EA, et al. A 10-year Review of the Clinical Presentation and Treatment Outcome of Asherman's Syndrome at a Center with Limited Resources. Ann Med Health Sci 2015; 5: 442-446.
- Conforti A, Krishnamurthy GB, Dragamestianos C, et Intrauterine adhesions after open myomectomy: an audit. European Journal of Obstetrics & Gynecology and Reproductive Biology. 2014; 179: 42-45.
- Ozumba B, Ezegwui H. Intrauterine adhesions in an African International Journal of Gynecology and Obstetrics. 2002; 77: 37-38.
- Gambadauro P, Gudmundsson J, Torrejon Intrauterine adhesions following conservative treatment of uterine fibroids. Obstetrics and Gynecology International. 2012; 853269.
- Muffly T M, Ridgeway B, Abbott S, et Small bowel obstruction after hysterectomy to treat benign disease. Journal of Minimally Invasive Gynecology. 2012; 19: 615-619.
- Angenete E, Jacobsson A, Gellerstedt M, et Effect of laparoscopy on the risk of small-bowel obstruction: a population-based register study. Archives of Surgery. 2012;147: 359-365.
- Tao Z, Duan Expression of adhesion-related cytokines in the uterine fluid after transcervical resection of adhesion. Zhonghua Fu Chan Ke Za Zhi. 2012; 11: 734-737.
- Chen Y, Chang Y, Yao Role of angiogenesis in endometrial repair of patients with severe intrauterine adhesion. Int J Clin Exp Pathol. 2013; 11: 1343-1350.
- Yu D, Wong YM, Cheong Y, et al. Asherman syndrome-one century Fertil Steril. 2008; 11: 759-779.
- Schenker JG, Margalioth Intrauterine adhesions: an updated appraisal. Fertil Steril. 1982; 11: 593-610.
- Berman Intrauterine adhesions. Semin Reprod Med. 2008; 26: 349-355.