Has Knowledge Influenced Right Choice? Assessing the Feeding Practices for Infants of HIV Positive Mothers in a Rural Northern Nigeria
Author'(s): Uzoma Kizito Ndugbu1* and Chizoba Elsie Madukwe2
1Public Health Department, School of Health, Federal University of Technology, PMB 1526 Owerri, Imo State. Nigeria.
2Paediatrics, Post Basic Studies, University of Port Harcourt Teaching Hospital, Choba, Rivers State. Nigeria.
*Correspondence:
Uzoma Kizito Ndugbu, Public Health Department, School of Health, Federal University of Technology, Imo State. Nigeria, Tel:+234-8032654963; E-mail: kizykn@gmail.com.
Received: 27 January 2018; Accepted: 02 March 2018
Citation: Uzoma Kizito Ndugbu, Chizoba Elsie Madukwe. Has Knowledge Influenced Right Choice? Assessing the Feeding Practices for Infants of HIV Positive Mothers in a Rural Northern Nigeria. Gynecol Reprod Health. 2018; 2(2): 1-6.
Abstract
Background: Infant feeding is vital and a key determinant of good nutrition and health status, survival and development. Breast feeding is universal and socio-culturally acceptable method of child feeding. Breast milk is nutritionally balanced and provides immunity against diseases. However, breast milk can transmit HIV from mother to child. This has posed public health dilemma. A lot of work has been done on HIV including MTCT but there remains a dearth of information related to appropriate feeding for infants of mothers infected with HIV, especially in the African rural setting.
Objective: The study was aimed at assessing infant feeding practices and viable breast milk alternatives for infants born to HIV positive mothers and how the knowledge of MTCT influence the choice of such practices in a rural community in Northern Nigeria.
Method: Descriptive cross-sectional study design employing both quantitative and qualitative methodologies was used. Stratified sampling was used to sample 5 health facilities out of 16 to be included in the study. 111 HIV positive mothers with children aged 0-12 months attending services in the sampled health facilities were randomly assigned numbers and systematically sampled to participate in the study.
Results: Maternal knowledge on MTCT of HIV was high (66.7%) in the study area. However, this had no association with maternal choice of infant feeding practice. The choice of alternative infant feeding practice was rather influenced by a number of factors among them; stigma and discrimination, belief about HIV transmission from mother to child (P=0.05) and HIV has no cure (P=0.03). Cow’s milk is the most preferred infant feeding option (99.1%) followed by commercial infant formula (96.4%).
Conclusion: The choice of infant feeding practice is not associated with level of maternal knowledge of MTCT of HIV. Commonly used infant feeding options include cow milk, porridge and commercial formula. World Health Organization guidelines on infant feeding in HIV recommends exclusive breast feeding to infants for six months.
Keywords
Introduction
The place of infant feeding in child development and survival is so vital that it is considered an essential key determinant in the first year of life. Breastfeeding is a universal socio-culturally acceptable, nutritious way to feed an infant and provides immunity [1]. However, the emerging of HIV/AIDS epidemic and the recognition that HIV positive mothers can transmit the virus to their babies through breast milk precipitated a terrible public health dilemma in countries with a high incidences of HIV. This situation is more worry in countries like Nigeria where breastfeeding is a norm and essential for child survival [2]. Mother to child Transmission (MTCT) of HIV is the primary way that children get infected and without prevention, over 40% of the children born to HIV positive mothers get infected [2]. Of those infected through MTCT, over 66% get infected during pregnancy and deliveries, while 33% get infected through breast-feeding [2]. For children under 2 years of age, this is almost the only way they get infected [3].
Human immune-deficiency virus (HIV) is a chronic, health problem with symptoms appearing anytime from several months to years. HIV is found among all known populations of the world, including the embryonic population (unborn babies) and the breastfed babies. World Health Organization, [4] stated that more than twelve million people worldwide had died of AIDS, while another 3.6 million of people are already infected with HIV, with a daily infection rate of over 16,000 people globally. It is estimated that 35% of under-five mortality is due to HIV and AIDS [5].
Prevention of mother-to-child transmission (PMTCT) of HIV is an important intervention in the prevention and control of HIV and AIDS to reduce child mortality and increase the rate of child survival. Mother-to-child transmission (MTCT) of HIV interventions requires more than provision of drugs and commodities. Systems must be strengthened and communities need to be prepared for this program. Therefore, commitment to providing a range of core MTCT interventions is required to reduce the incidence of MTCT of HIV. This would require a complete package of health care including maternity and family planning services with increased antenatal care, voluntary counseling and testing (VCT) for HIV, possible use of antiretroviral drugs and use of safe alternatives to the infected mother’s breast milk [6]. A culturally acceptable, low cost approach to infant feeding is essential to prevent breast milk HIV transmission [7]. In countries not affected by HIV, improving infant feeding can reduce mortality by up to 19%. The impact could be greater in HIV affected populations if interventions that reduce HIV transmission through breast feeding could be successfully linked to strategies that improve infant feeding practices.
However, this is confounded by complexity of identifying most appropriate infant feeding practices that fits household and social circumstances of mothers. World Health Organization [8] recommends that in light of the effectiveness of ARVs, HIV infected mothers should continue breast feeding the infant until twelve months of age. This capitalizes on the maximum benefit of breast feeding to improve the infant’s chances of survival while reducing the risk of HIV transmission. The guideline also recommends to national health authorities to promote a single infant feeding practice as a standard of care.
The information about other practices should be made available. This calls on governments and donors place responsibility on them to increase commitment to and resources for improving infant feeding practices in HIV affected populations. The investment should be targeted to effectively prevent infants becoming infected with HIV through breast feeding, improve HIV free-survival of infants and achieve international developments goals, such as the now Sustainable Development Goals (SDGs) and those set by United Nations General Assembly Special Session on HIV and AIDS (UNGASS).
Truth is, HIV and AIDS is a not just a national disaster but a global pandemic. Multidisciplinary efforts are needed to curb this problem that is reversing trends of child survival and development. Though, efforts to this regard have been through campaigns, supply of relatively cheap or free anti-retroviral drugs and other preventive measures such as prevention of mother to child (PMTCT) [2]. Indeed, studies have shown that HIV could be transmitted from infected mothers to their nursing babies; such transmission is possible through feeding options [9,10]. Such mode of transmission has increased the likelihood of infants being infected and has attracted attention globally.
FMOH [11] observed that HIV infection among infants has been on the increase and that it is one of the major causes of childhood death. The report further pointed out that this case is worsened by the feeding options adopted by HIV infected mothers. To emphasize this finding, Ajayi, Hellandendu and Odekunle [12] in their study observed that more than 90% of HIV infected infants were from mother to child during birth or breast feeding. Hence feeding option is one of the critical modes of HIV transmission from mothers to infants. Despite the guide by FMOH and observations, the researcher has noticed in clinical practice, that there seem to be misconceptions by HIV infected mothers on infant feeding options, especially given the means available. Granted that infants contract HIV from their mother’s during birth or during breast feeding, there is the growing awareness about the available infant feeding options adopted by HIV positive mothers, as this then is the case, what socio-economic factors influencing the choices of feeding options adopted by HIV positive mothers? Especially, as a successful approach to alternative feeding would be a less expensive intervention compared to ARV drugs used to minimize the viral load of HIV and improve the quality of life.
This research thus is aimed at to examining the socio-economic factors influencing the choices of infant feeding practices among HIV positive mothers in Zing, Taraba State, Nigeria.
Materials and Methods
Taraba State is situated between latitude 6*25’N and longitude 9*30’E to 11*45’E with tropical continental type of climate. With a land area of about 62,291km2 [13], Taraba is the second largest in Nigeria having a total population of over 2.4 million people according to the 2006 population census. Its location is on the mountain ranges in the Eastern borderland of Nigeria separating Nigeria and Cameroon. It is bordered on the west by Nassarawa and Plateau States, to the north by Bauchi and Gombe States, and by Adamawa State to the northeast. It shares its southwestern boundary with Benue State.
Taraba State’s location is disadvantaged with regard to HIV/AIDS prevalence, not only as it shares close boundaries with regions that have highest rates of the virus (Benue, Plateau States of Nigeria, and Bamenda region of Cameroon) [14], but also that the increasing rate of the pandemic is hindering its development. This is especially so in Zing town with a prevalence rate of 5.6% among pregnant women [15], which is why, it became a study area. Zing town, with an area of 1.030km2 has a population of 127,363 at the 2006 census; 98% whom are predominantly of the Mumuye tribe.
Study Design
Cross-sectional descriptive study design was used to collect qualitative and quantitative data. This design was preferred because it was relatively cheap and had ability to collect diverse data within a short period required analysing cause-effect relationships in representative subset of a population.
Study Population
The study involved HIV positive mothers aged 15-49 years who were registered and were attending Anti Retro-Viral Therapy (ART) or attending support group meetings in designated health facilities from November 2017-March 2018 in Zing town. Health workers from the health facilities which offered PMTCT, traditional birth attendants (TBAs) and community midwives were the key informants.
Inclusion criteria
The respondents who were eligible to participate in the study included mothers of reproductive age bracket (15-49 years) aware of their HIV sero-status, had a child aged 0-12 months and were residents of Zing for a period not less than 6 months. Respondents who gave verbal informed consent participated in the study.
Exclusion criteria
Ineligible respondents included those who were young or older than the framed age bracket (15-49 years), had no infant or had a child over 12 months of age. Respondents and /or their children who were sick with opportunistic infections (OI) and unable to participate in the interview were excluded. Those who were non- residents had stayed in the study area for less than 6 months or were excluded from the study. Respondents who did not give verbal informed consent were also excluded from the study.
Sample size determination
The study employed multistage sampling. In the first step, stratified sampling was used to sample 5 health facilities out 18 to be included in the study. The health facilities were categorized into three strata as primary, secondary and tertiary care. This was based on government of Federal Ministry of Health classification of health facilities.
Each health facility in each stratum was assigned a random number. The numbers were written on a piece of paper, folded and mixed up by stratum for sampling. Two health facilities in each stratum were sampled using simple random sampling. The tertiary stratum had only 1 health facility, which was the specialist hospital. This had 1 chance of being sampled. A list of HIV positive mothers/ clients enrolled for HIV continuum of comprehensive ART care services in each health facility that was sampled was provided. The client enrollment/registration numbers assigned by each sampled health facility was used. The respondents who met the inclusion criteria were systematically sampled and recruited in the study.
Sample size
The district HIV prevalence among pregnant women was 7.4% (DHS, 2007). Assuming standard error of 5% and confidence interval (C.I) of 95%, the sample size for this study was determined using Fisher’s formula [16]:
Where:
n: Is the sample size
Z: The value corresponding to the normal deviate (confidence limit) taken as 1.96 at 95% confidence level
p: Proportion of HIV infected women in the study population
q: Proportion of women not infected with HIV in the population
(1-p from infinite population)
d: Is the acceptable degree of accuracy (SE) desired (0.05)
n = Z2pq = (1.96 x 1.96) x 0.074 x 0.926 = 105 Subjects d2 0.05
x 0.05
Allowing fall out rate of 10% the study targeted 115 respondents.
Ethical Consideration
An ethical clearance was obtained from the research ethic committee of the Ministry of Health, Jalingo. Verbal informed consent was sought from 111 respondents after being informed of the objective and design of the study before an interview was conducted. Confidentiality and anonymity was assured to respondents who participated in the study.
Results
Socio-deomgraphics
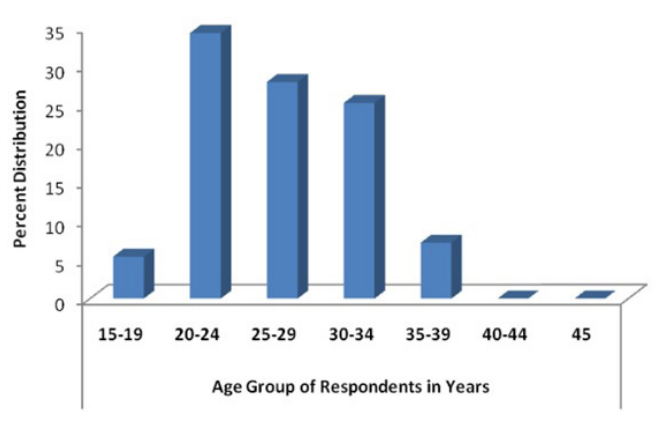
Figure 1: Distribution of respondents by age.
A total of 111 HIV positive mothers of reproductive age bracket 15-49 years with infants aged 0-12 months participated in the study while 4 mothers dropped from the study. The highest proportion of mothers (34.2%) was in age group 20-24 years while 5.4% were teenagers. The mean maternal age was 26.7+5.23 years (S.D=5.23).
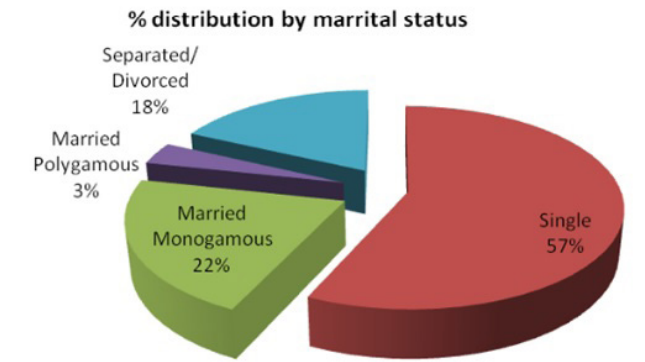
Figure 2: Distribution of respondents by marital status.
The study found that more than half (56.8%) of the respondents were single while 21.6% were in monogamous marriage relationships. The rest were either separated/ divorced or in polygamous marriage relationships. Single mothers were frequent within the age group 20-24 years (21.6%). The average household size in monogamous, polygamous and separated marriage relationship was 5.1+1.3 (95% CI=2.6 - 7.7).
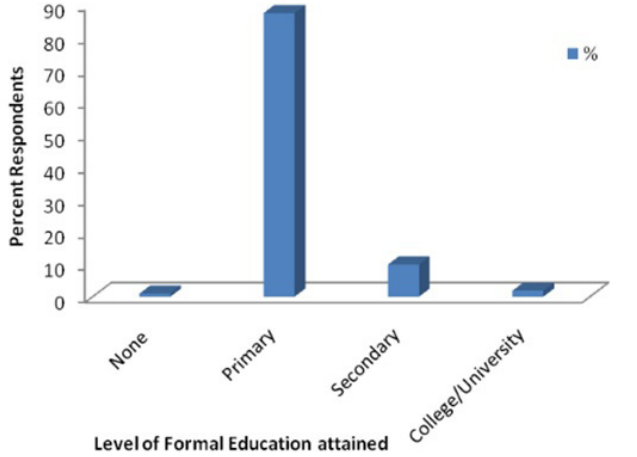
Figure 3: Level of Formal Education attained by respondents.
From this study 97 (87.4%) of respondents attained primary level education while 10 (9.9%) had secondary level of education. This revealed that about 1 in every 10 respondents involved in the study had secondary education. Those who had attained college/ university education were 13 (1.8%)
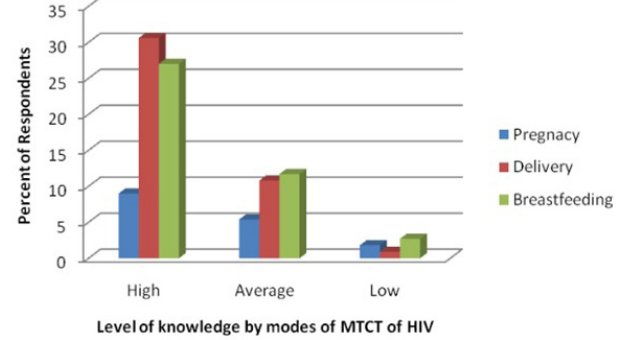
Figure 4: Level of knowledge of occurring modes of MTCT of HIV.
This study recorded the level of knowledge among respondents on a three scale rating with one being the lowest, two as average and three as highest. Rating of knowledge was based on respondents level of understanding on general facts about HIV, whether a child can get HIV, timing and of transmission and prevention of HIV from mother to child that’s during pregnancy, delivery and breast feeding. A total of 47 (42.3%) respondents knew that HIV could be transmitted from mother to child during delivery, 46 (41.5%) during breast feeding and 18 (16.2%) in pregnancy period. Analysis on prevention of MTCT of HIV revealed that 95% of the respondents knew that it was possible. Cross analysis on cure revealed that about 68.5% of the respondents knew that HIV/AIDS kills and has no cure while 28.8% said it could be cured and 2.7% did not know.
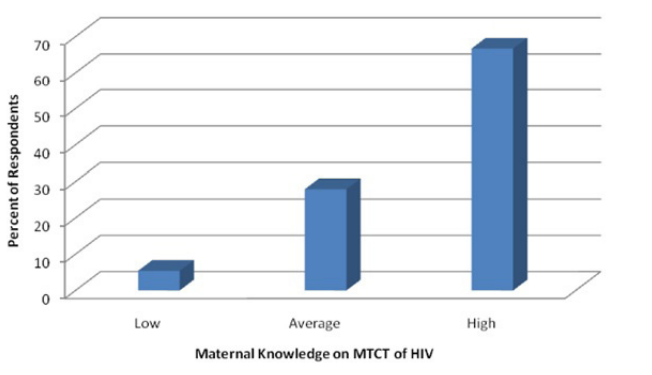
Figure 5: Level of Maternal Knowledge of MTCT of HIV.
The study showed that 66.7% of the respondents had high level of knowledge while 5.4% had low level of knowledge. The bivariate analysis using Chi-square showed no association between the level of maternal knowledge (P=0.09) and choice of infant feeding practice (P=0.05, 95% CI). Similarly, the level of education attained and respondents’ knowledge on MTCT of HIV was not statistically associated. Analysis of respondents’ exposure to information received in different modes and sources such as health education, counseling and information education & communication materials (IEC) (P=0.06) was also not associated with choice of infant feeding practice.
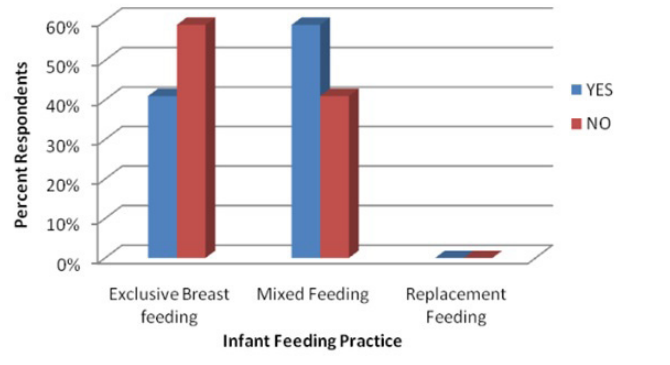
Figure 6: Distribution of Infant feeding practices.
Results of bivariate chi-square analysis showed how level of acceptability (P=0.05) of breast feeding as an infant practice among respondents. The reasons provided were that breast milk has nutritional value, provides immunity, readily availability, social-culturally viable and economically feasible. It was also found out that 72 (64.5%) of the respondents involved in the study had ever breast fed their infants. A small number (5.5%) initiated infants to breast milk within one hour after birth. Frequency of breast feeding varied with respondents. A total of 62 (55.6%) reported having breastfed their infants on demand while, 11.1 % breastfed 4 times or less and 33.3% breastfed at least 5 times a day. In regard to exclusive breast feeding (EBF) for the first 6 months of infant’s life, 37 (40.6%) fully practiced EBF. Among respondents interviewed to determine the period taken for continued breast feeding children 6-12 months, (92.7%) reported having previously breast fed their infants for less than 12 months while only 7.3% breast fed for at least 12 months.
The results indicated that 59% (N=111) of the respondents in the study area practiced mixed feeding (P=0.05). Breast feeding was done in combination with other foods and fluids. The foods commonly fed to infants alongside breast milk included among others porridge, animal milk and mashed foods. Respondents (63.1%) introduced such foods to infants at the age of 4-6 months of infant’s life. Reasons behind practicing mixed feeding included among others; insufficient breast milk (85.7%), onset of another pregnancy (4.8%), mothers’ engaged in economic or social activities away from home/ child and deliberately accustoming the baby to family foods (4.8%).
Respondents in this study indicated that replacement feeding was expensive, not feasible and therefore not sustainable in their low income context. Focus group discussion with mothers indicated that this was accessible by families which had stable or reliable income. Issues around inadequate technical knowhow on preparation, sanitation and hygiene emerged in the study community. Results of Chi-square analysis showed that expect for the cost, commercial formula (P=0.05) was acceptable to respondents as safe and nutritious infant replacement feeding option in the context of HIV. This method was preferred by 96.4% respondents.
Discussion
Age, marital status, and education status are socio demographic characteristics which can influence individuals’ values, knowledge, attitudes, behaviour and practices. These findings are in agreement with the study of Coutsoudis [17] and Coutsoudis, Coovadia, Pillary and Kuhn [18] who found out that religious beliefs, occupation, marital status and age influence the choice of infant feeding options. However, findings disagree with that of Young et al., [19] and Bekere et al., [20] were socio-demographic factors were seen having or no influence.
Also, findings of this study revealed that 16.2% of the respondents knew that HIV could be transmitted from mother to child in pregnancy, 42.3% during delivery and 41.5% during breast feeding. This implied that all respondents knew that MTCT of HIV is largely through vertical transmission. Awareness on HIV and AIDS in the town is high (99.8%), however, the level of knowledge on MTCT of HIV has not been widely documented, even though its knowledge was high 66.7%. A study by Oguta et al., [21] in Homa Bay Western Kenya reported low knowledge on MTCT of HIV. On the contrary, the level of maternal knowledge on MTCT of HIV had no significant effect on infant feeding practices. The results point out that breast feeding is deep rooted and most preferred in the rural setting. This applies across to all people regardless of knowledge on their sero-status.
Furthermore, UNAIDS [22] documented that mixed feeding is not recommended since it increases risk of HIV transmission through breast feeding. Results of this study revealed that respondents practiced mixed feeding even after receiving counselling and health talk at health facility. Some fears lied in not breast feeding despite the high level of knowledge. Despite the high level of maternal knowledge, appropriate and recommended infant feeding still remain a challenge. Although, literature indicated that mixed feeding damages the intestinal lining of the gut in infants, leading to an increased risk of HIV transmission through breast milk [23], the majority of the respondents practiced mixed feeding. This result matched with the study conducted at Dares Salaam which showed exclusive breast feeding rates among HIV positive mothers was high among infants from birth, and this go decreasing rapidly until six months of age [24,25].
Transmission was lower in exclusively breastfed infants because it maintains a healthy gut epithelium, which acts as a viral barrier, and that breast milk contains immune factors which have anti-viral and anti-HIV effects in vitro [4,26].
Conclusion and Recommendations
Infant feeding is critical in early life and key determinant to child survival and development. This is more challenging in context of HIV due to vertical transmission from mother to child. It was concluded that mothers in Zing have high knowledge MTCT of HIV. However, there was general poor adherence to WHO [4] guidelines. There is need to sensitize communities to adhere to infant feeding guidelines and ART treatment regimes in context of HIV to prevent mother to child infection. As such, the choice of maternal infant feeding practices is not influenced by the level of maternal knowledge.
This study recommends the strengthening of MTCT support systems beyond care at health facility level to enhance maternal knowledge and practice. Also, given that mixed feeding to infants before six months increases risk of MTCT of HIV; there is need, then, to intervene through health education, counselling and sensitization to health workers and mothers on the importance of adherence to WHO recommended guidelines.
Finally, there is need to intensify sensitization on vertical transmission of HIV and associated risks to mothers attending MCH services in the health facilities. Health care providers need to intensify health and nutrition education, voluntary and confidential counselling and testing.
References
- Efforts to prevent mother to child transmission of HIV/AIDS; an overview of US Agency for international development program, Washington DC. 2001.
- Abiona TC, Onayade AA, Ijadunola KT, et al. Acceptability, feasibility and affordability of infant feeding options for HIV- infected women: A qualitative study in south-west Nigeria. Maternal Child Nutrition. 2006; 2: 135-144.
- Chopra M, RollinsN. Infant feeding in the time of HIV: rapid assessment of infant feeding policy and programs in four African countries scaling up prevention of mother to child transmission Arch Dis Child. 2008; 93: 288-291.
- World Health HIV transmission through breastfeeding. A review of Available Evidence, Genva. WHO. 2011.
- Collaborative study team on the role of Breastfeeding on the prevention of infant mortality. Effect of breastfeeding on infant and child mortality due to infectious diseases in less developed countries: a pooled analysis. Lancet. 2009; 335: 451-455.
- Sethuraman K, Hammond W, Hoang MA, et al. Challenges for Safe Replacement Feeding among HIV-Positive Mothers in Vietnam: A Qualitative Study of Mothers, Fathers, Health Care Providers, and Other 2011.
- Mohammed A, Shehu AU, Aliyu AA, et al. Infant feeding options, practices and determinants of feeding practices among HIV sero-positive mothers in Abuja, Nigerian medical journal. 2008; 51: 14-17.
- World Health Organization (WHO). Interagency Task Team on prevention of HIV infection in pregnant women: Guidance on global scale up of the prevention of mother-to-child transmission of HIV. Towards universal access for women, infants and young children and eliminating HIV and AIDS among Geneva: WHO. 2006.
- Moses A, Chama S, Udo S, et al. Knowledge, attitude and practice of antenatal attendance towards PMTCT of HIV – infection in a tertiary health facility, Northeast-Nigeria. The Internet Journal of Third World 2009; 8: 580-594.
- Matji JN, Wittenberg DF, Makin JD, et al. Psychosocial and economic determinants of infant feeding intent by pregnant HIV-infected women in Tshwane/Pretoria. South African Journal of Child 2008; 2: 114-118.
- Federal Ministry of Health (FMoH). National Guidelines on prevention of mother-to- child transmission of HIV (PMTCT). Abuja, 2011.
- i AD, Hellandendu J, Odekunle F. Socio-demographic correlates of breastfeeding practices among mothers in kogi state, Nigeria, West African Journal of Nursing. 2008; 22; 28- 35.
- Oruonye The Geography of Taraba State, Nigeria. Fab Educational Books. 2010.
- Oruonye An assessment of the response to HIV/AIDS pandemic in Taraba State, Nigeria. J Geogr & Regl Plann. 2011; 4: 104-109.
- Family Health International (FHI). Report of Rapid Assessment in Selected LGAs in Taraba State, 2000.
- Fisher AA, Laing JA, Townsend Handbook for Family Planning Operations Research. Population Council, USA. 1991; 43-46.
- Coutsoudis A. Infant feeding dilemmas created by HIV: South African experiences. Nutrition Journal. 2005; 135: 956-999.
- Coutsoudis A, Coovadia H, Pillay K, et al. Are HIV- infected women who breastfeed at increased risk of mortality?. 2005; 15: 653-655.
- Young SL, Mdudua NN, MbuyaE, et al. Current knowledge and future research on infant feeding in the context of HIV: basic, clinical, behavioral, and programmatic Adv Nutr. 2011; 2: 225-243.
- Bekere A, Garoma W, Beyene Exclusive Breastfeeding Practices of HIV Positive mothers and its Determinants in Selected Health Institution of West Oromia, Ethiopia. J Nutr Food Sci. 2014; 4: 319.
- Oguta T, Omwega A, Sehmi J. Infant and young child feeding in emergencies (IFE) Kenya. 2004; 22-26.
- UNAIDS/WHO/UNICEF. HIV and Infant Feeding; A policy statement developed collaboratively by UNAIDS, WHO and UNICEF/UNAIDS; 2008.
- Manji KP. Breast Feeding and HIV Infection among Children Born to HIV Infected Mothers. Research report. 2011; 30-33.
- Coovadia HM, Rollins NC, Bland RM, et Mother-to- child transmission of HIV-1 infection during exclusive breastfeeding in the first 6 months of life: an intervention cohort study. Lancet. 2007; 369: 1107-1116.
- Muluye D, Woldeyohannes D, Gizachew M, et Infant feeding practice and associated factors of HIV positive mothers attending prevention of mother to child transmission and antiretroviral therapy clinics in Gondar Town health institutions, Northwest Ethiopia. BMC Public Health. 2012; 12: 240.
- Wahl SM, McNeely TB, Janoff EN, et al. Secretory Leucocyte Protease Inhibitor (SLPI) in Mucosal Fluids Inhibits HIV-1. Oral 1997; 3: 564-569.