Pregnancy Complicated with Dilated Cardiomyopathy: A Case Report
Author'(s): Sultana Aklima1*, Noor Sirajun2, Sultana Kawsar3, Alam Jahangir4 and Rajat Sanker Roy Biswas5
1MBBS, FCPS (Obs & Gynae), Assistant professor, Department of Obstetrics and Gynecology, Chattogram Maa Shishu O General Hospital, Chattogram, Bangladesh.
2 MBBS, FCPS (Obs& Gynae), Head of the Department, Obstetrics and Gynecology, Chattogram Maa Shishu O General Hospital, Bangladesh.
3 MBBS, MPH, Lecturer, Department of Community Medicine, Chattogram Maa Shishu O General Hospital, Bangladesh.
4MBBS, DCH, Registrar, Department of Pediatrics, Chattogram Maa Shishu O General Hospital, Bangladesh.
5 MBBS, MD (Internal Medicine), Asst. Professor, Department of Medicine, Chattogram Maa Shishu O General Hospital, Bangladesh.
*Correspondence:
Dr Aklima Sultana, House# 17, Lane # 10, Rd# 01, Block-H, Halishahar Housing Estate, Chattogram, Bangladesh, Tel: +881816350046.
Received: 04 February 2020; Accepted: 25 February 2020
Citation: Sultana Aklima, Noor Sirajun, Sultana Kawsar, et al. Pregnancy Complicated with Dilated Cardiomyopathy: A Case Report. Gynecol Reprod Health. 2020; 4(1): 1-3.
Abstract
Cardiomyopathy, a disease of the heart muscles, is difficult to manage and can lead to sudden cardiac death. Dilated cardiomyopathy, a form of cardiomyopathy, with recurrences in subsequent pregnancies, increases the morbidity and mortality of both mother and child. Here, we report a case of a 25-year-old woman with amenorrhea for 6 weeks and a history of dilated cardiomyopathy during her previous pregnancy. Despite the risks and associated complications with the disease, she willingly continued her pregnancy and underwent caesarian section giving birth to a premature alive baby. The aim of this case is to provide guidance on how to manage a patient with dilated cardiomyopathy throughout her pregnancy including antenatal, intranatal and postnatal care.
Keywords
Introduction
Peripartum cardiomyopathy (PPCM), also known as post-partum cardiomyopathy, is a rare type of heart failure that occurs during the last month of pregnancy or up to five months after giving birth [1]. From a cardiologist’s point of view, peripartum cardiomyopathy is defined as dilatation and failure of the left ventricle, that first developed during the third trimester of pregnancy or within the ‘first six months postpartum’ [2]. Previous cardiac problems may not be found in such patients and the cause of cardiomyopathy remains unknown. PPCM is a form of dilated cardiomyopathy (DCM), where the heart becomes enlarged and is unable to efficiently pump blood. Diagnosing DCM during pregnancy is difficult since the clinical features may mimic the symptoms of a normal pregnancy. Hence, identification of systolic dysfunction and left ventricular dilatation using echocardiography is diagnostic for DCM. Adverse cardiac events are more common in DCM complicated with pregnancy and worsens with subsequent pregnancies. Also, the prognosis is much worse than the non-pregnant counterparts [3]. Furthermore, fetal and neonatal complications are more common in pregnant women with DCM. As a result, early termination of pregnancy is an option that can be taken to prevent further deterioration of cardiac function by evading the ‘stress and burden of pregnancy’ [4].
The following case study deals with the management and successful delivery of a second child to a diagnosed DCM mother whose pregnancy had been complicated due to the disease.
Case
A 25-year-old woman came with amenorrhea for six weeks. Her last menstrual period was on 28/1/2018and her expected date of delivery was 5/11/2018. This was her second pregnancy (Gravids-2, Para-1+0).
Two years back, in June 2016 she had her first child through normal vaginal delivery. Her first pregnancy was uneventful and there were no known pregnancy complications during that time. However, 20 days after delivery, she came to the out-patient department with respiratory distress and palpitation. Suspecting a cardiac cause, an echocardiography was done. Results showed global hypokinesia with an ejection fraction of 37%. She was thus diagnosed with peripartum cardiomyopathy. Since then she has been receiving a cardiac glycoside (Digoxin) and a potassium sparing diuretic (Spironolactone) for treatment. Further, she was also advised never to conceive again. Now, two years later, against doctors’ advice, she conceived again.
Antenatal period
Patient came for her 1st antenatal checkup in her 6th week of pregnancy. She had stopped taking her medications for cardiomyopathy before her visit, once her pregnancy test came to be positive. After her checkup she was advised to consult with a cardiologist. An echocardiography was done during the 9th week of her pregnancy. The echocardiogram showed normal findings, with an ejection fraction of 51% and patient was advised that she could continue with her pregnancy if she desired. She was prescribed with loop diuretics (Frusemide+ Spironolactone), an antiplatelet drug (Aspirin) and a β- blocker (Bisoprolol) for use throughout the pregnancy up till a week before her expected date of delivery. In the meantime, she continued to come for regular antenatal checkups. On her 24th week of pregnancy an anomaly scan was done that appeared to be normal. During her 26th week of pregnancy, patient began to complain about mild respiratory distress. An ECG was done the following day and her cardiac status was within normal limits. She was referred to her cardiologist, who advised her to continue with her medications. No further echocardiography was done that day.
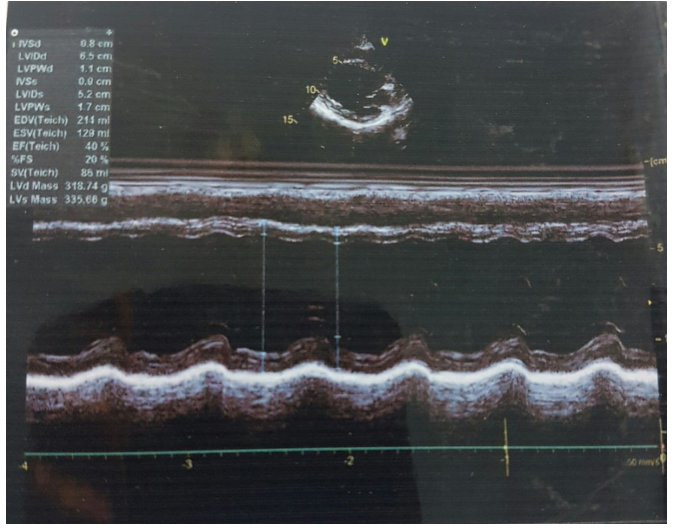
Figure 1: Antepartum Dilated Cardiomyopathy.
Patient came for checkup in her 29th week of pregnancy and on 34th week of pregnancy. Patient was fine during both checkups. Another echocardiography was done on a routine basis in her 34th week of pregnancy. This time the echocardiographic findings were consistent with dilated cardiomyopathy, with grade 1 diastolic dysfunction. Ejection fraction was 40%, but patient did not show any symptoms (Figure 1).
She was hospitalized at 36 weeks of pregnancy with a plan for undergoing caesarian section.
Intra natal period
Patient did not undergo labor. A medical board was set up and a joined consultation involving a cardiologist, an obstetrician and an anesthesiologist was conducted to discuss the risks involved. Patient underwent caesarian section and low dose bupivacaine was used for spinal anesthesia. A male child weighing 1.9kg was born. Despite patient counselling for tubal ligation it was refused. Child was referred to neonatal ICU due to prematurity and low birth weight.
Post-natal period
The baby was released from NICU after a week’s stay there and simultaneously the mother was discharged with an advice to consult with her cardiologist. On discharge, patient was prescribed with carvedilol and vitamin B complex. Another week later she was advised to undergo one last echocardiography to check the status of her ailing heart. Echocardiographic findings were consistent with dilated cardiomyopathy with an ejection fraction of 36.84%, and moderate left ventricular systolic dysfunction (Figure 2). Patient came for follow up with both obstetrician and cardiologist two weeks and four weeks after delivery.

Figure 2: Postpartum Dilated Cardiomyopathy.
Discussion
Many articles were published discussing the adverse effects of dilated cardiomyopathy and how pregnancy can have a negative impact on such patients. One study (Grewal, et al., 2010) implies that pre-pregnant characteristics of the patient’s disease can help predict which women would be at higher risk. Another case study [4], counselled two women with peripartum cardiomyopathy in their first pregnancy that they could reconceive if their dobutamine stress echocardiography (DSE) performance test before conception came out to be normal. These women were at lower risk of developing cardiac complications during pregnancy and as follows, successfully delivered healthy babies without any complications during their pregnancy. This case is different since our patient came to us after conception and hence, it was not possible to conduct any test, or accurately say the pre-pregnant characteristics of the patient. As a result, managing this patient was comparatively difficult and quite risky.
Angiotensin converting enzyme inhibitors and angiotensin receptor blockers were never prescribed to this patient and hence, chances of teratogenicity in the infant due to these drugs were avoided. Nevertheless, patient did receive digoxin and spironolactone on a regular basis prior to conception until she voluntarily stopped taking the medications once she realized she was pregnant. While low dose aspirin is considered to be safe for the child, beta blockers and loop diuretics (frusemide and spironolactone) carry their own risks during pregnancy7. Even though diuretics are said to affect the plasma volume expansion during pregnancy, studies have found no correlation with a negative effect on fetal growth [7]. And since the benefits of these drugs outweighed the risks, they were used.
Echocardiography was used as the single most effective tool to assess the condition of the heart during pregnancy. The first echocardiography after conception showed an ejection fraction of 51%. Although it was below the normal limit of 60%, the patient was told she could continue with her pregnancy. However, as her pregnancy progressed, her ejection fraction began to fall, and it reached 38.5% in the last echocardiography done after her delivery. Despite a normal delivery the previous time, patient had to undergo a caesarian section this time to prevent further deterioration of heart function due to the stress of vaginal delivery.
Conclusion
Dilated cardiomyopathy is a life-threatening complication in pregnancy and patient should be properly counselled regarding its morbidity and mortality. In women with a history of peripartum cardiomyopathy, subsequent pregnancies may be associated with worse fetal and maternal outcomes such as prematurity of child, heart failure or even death of the mother [9]. Even after this if patient reconceives, she should have focused antenatal care. Cardiologist consultation should be taken during pregnancy, in labor and puerperium. As there is a chance of premature delivery, special neonatal care should be provided to the premature infant. Provided timely investigations, proper treatments and regular follow ups are adhered to, safe delivery of a child to a mother with DCM is a possibility.
Acknowledgements
This article was presented in the South Asia Federation of Obstetrics and Gynaecology (SAFOG) conference in 2019 that was held in Bangladesh.
References
- Khan MAM, BanooH, Ahmed SS. Peripartum Cardiomyopathy. Medtoday. 2013; 25: 96.
- O'Connell, John B, Costanzo-Nordin, et al. Peripartum Cardiomyopathy: Clinical, Hemodynamic, Histologic and Prognostic J Am Coll Cardiol. 1986; 8: 52-56.
- Grewal J, Siu SC, Ross HJ, et al. Pregnancy Outcomes in Women With Dilated Cardiomyopathy. J Am Coll Cardiol. 2010; 55: 45-52.
- Katsuragi S, Omoto A, Kamiya C, et al. Risk factors for maternal outcome in pregnancy complicated with dilated cardiomyopathy. J Perinatol. 2012; 32: 170-175.
- Van Tintelen JP, Pieper PG, Van Spaendonck- Zwarts, et al. Pregnancy, cardiomyopathies and genetics. Cardiovasc Res. 2014; 101: 571-578.
- Al Bannay R, Husain A, AlJufairi Z. Peripartum cardiomyopathy, what if your patient plans to reconceive? Clinical case reports. 2017; 5: 753.
- Al-Balas Mosa’b, Bozzo Pina, Einarson Adrienne. Use of diuretics during pregnancy. Mother risk. 2009; 55: 44-45.
- Neal K Lakdawala, Jeffery R Winterfield, Birgit H Funke. Dilated Cardiomyopathy. Circ Arrhythm Electrophysiol. 2013; 6: 228-237.
- Elkayam Uri, Tummala Padmini P, Rao Kalpana, et al. Maternal and fetal outcomes of subsequent pregnancies in women with peripartum cardiomyopathy. N Engl J Med. 2001; 344: 1567-1571.