Sizes, Numbers and Distribution of Uterine Fibroids Enucleated At Laparoscopic Myomectomy from Nigerian Women with Primary or Secondary Infertility
Author'(s): Abayomi Ajayi1, Bamgboye M. Afolabi2*, Victor Ajayi1, Oluwafunmilola Biobaku1, Ifeoluwa Oyetunji1, and Happiness Aikhuele1
1Nordica Fertility Centre, 106 Norman Williams Street, Ikoyi, Lagos, Nigeria.
2Health, Environment and Development Foundation, 34 Montgomery Road, Yaba, Lagos, Nigeria.
*Correspondence:
Bamgboye M. Afolabi, Health, Environment and Development Foundation, 34 Montgomery Road, Yaba, Lagos, Nigeria, Tel: +234 (1) 291 6562; E-mail: bmafolabi@heendef.org.
Received: 01 May 2017 Accepted: 03 June 2017
Citation: Abayomi Ajayi, Bamgboye M. Afolabi, Victor Ajayi, et al. Sizes, Numbers and Distribution of Uterine Fibroids Enucleated At Laparoscopic Myomectomy from Nigerian Women with Primary or Secondary Infertility. Gynecol Reprod Health. 2017; 1(1): 1-8.
Abstract
Background: Fibroids are the commonest benign gynaecological tumors affecting only females and laparoscopic myomectomy is the modern management because of its various advantages, especially among women who still desire retention of their fertility.
Materials and Methods: This is a retrospective review of 31 infertile patients who had laparoscopic myomectomy (LM) from January 2010 to December 2014 at Nordica Fertility Center. Information on socio-demographic characteristics such as age, body mass index and duration and type of infertility, marital status and parity were recorded. For the purpose of this paper, clinical data such as number of miscarriages, uterine size, site, size and number of fibroids were also noted. Data were analyzed using STATA 13 statistical software. P-value of 0.05 and below was regarded as level of acceptable statistical significance.
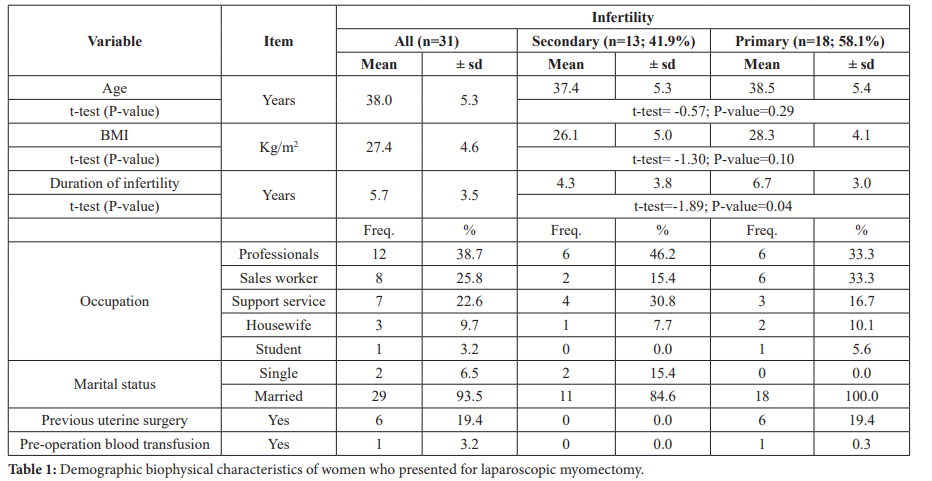
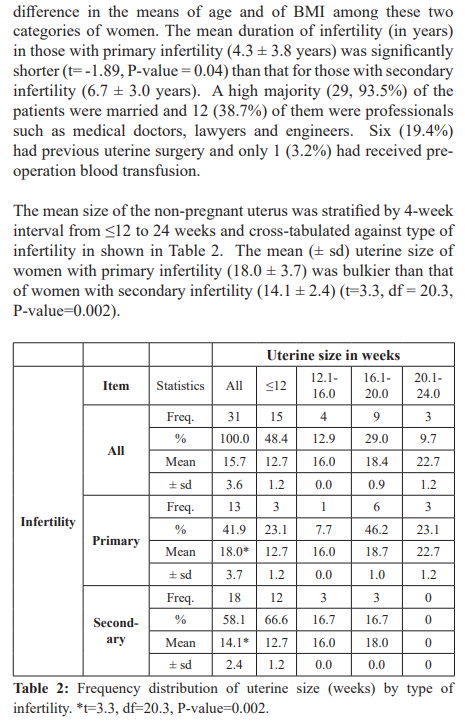
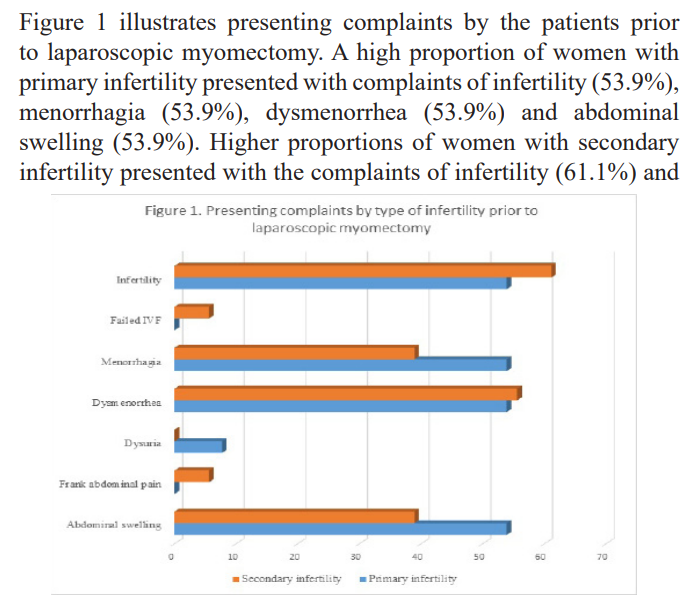
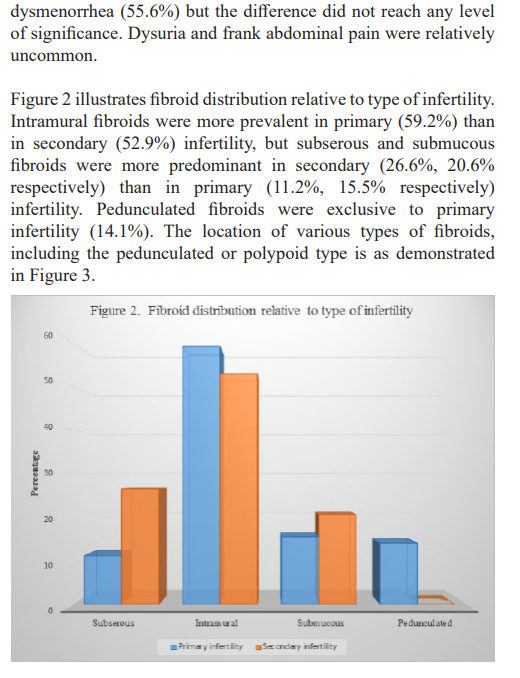
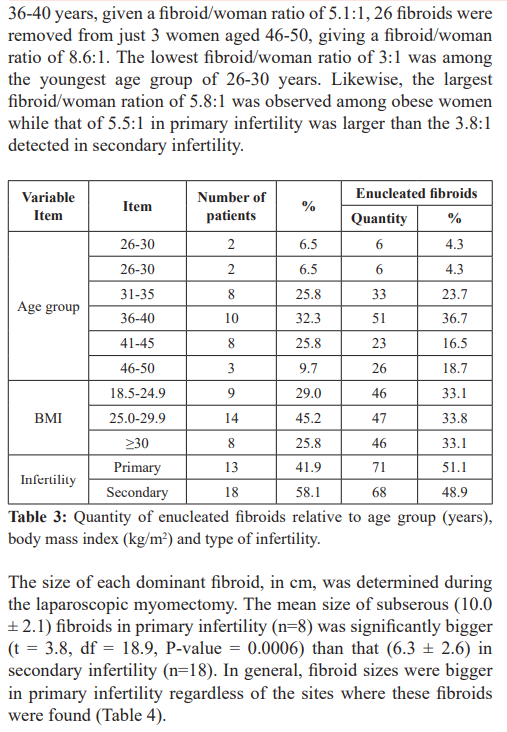
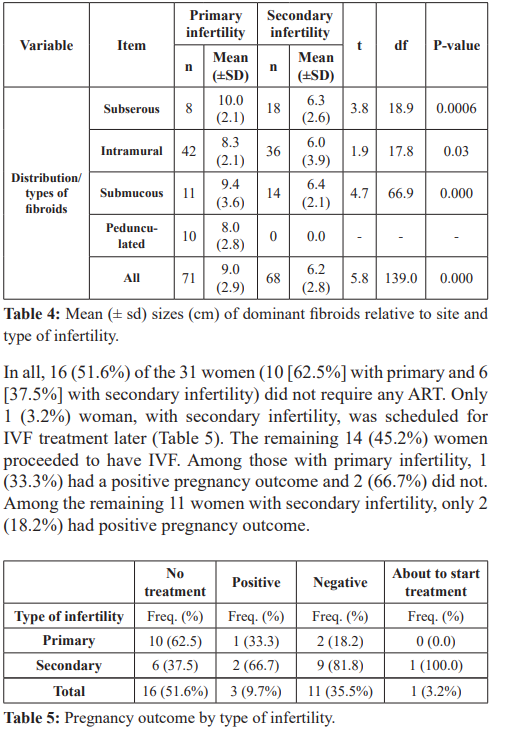
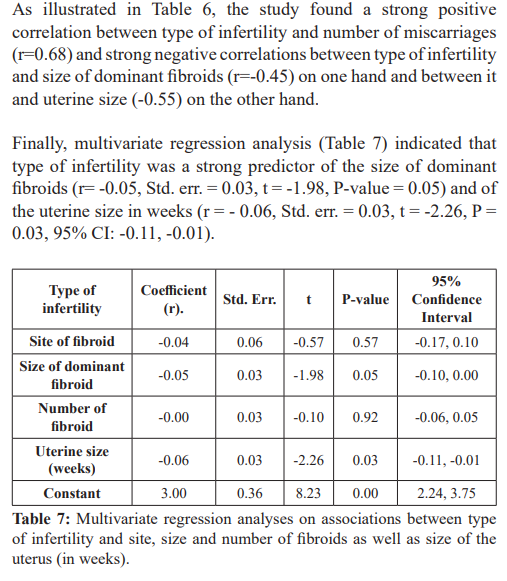
Results: A total of 31 women presented with fibroid for laparoscopic myomectomy. Their means (± sd) of age (years), Body Mass Index (kg/m2) and years trying to conceive (TTC) were 38.0 (5.3), 27.4 (4.6) and 5.7 (3.5) respectively. Among the patients, 13 (41.9%) and 18 (58.1%) presented with primary and secondary infertility respectively, 12 (38.7%) were professionals, 29 (93.5%) were married and 6 (19.4%) had previous uterine operation. The non-gravid uterus was significantly bulkier (weeks) in primary (18.0 ± 3.7) than in secondary (14.1 ± 2.4) infertility. Most prevalent symptoms were dysmenorrhea (53.9%,55.6%), menorrhagia (53.9%, 38.9%) and abdominal swelling (53.9%, 38.9%) respectively. Intramural fibroids were most common in both groups of women while pedunculated fibroid was exclusive to primary infertility. Highest fibroid /woman ratio of 8.7:1 was observed among women aged 46-50 years. Intramural fibroids were significantly bigger in primary than in secondary infertility (t = 1.9, P-value = 0.03). Type of infertility was a strong predictor of the size of the non-gravid uterus with fibroids (r = -0.06, Std. err. = 0.03, t = -2.26, P = 0.03, 95% CI: -0.11, -0.01).
Conclusion: Women with primary infertility are prone to larger fibroid size and tend to have more fibroids per person while those with secondary infertility are more likely to have fibroid located in sub serous site.
Keywords
Introduction
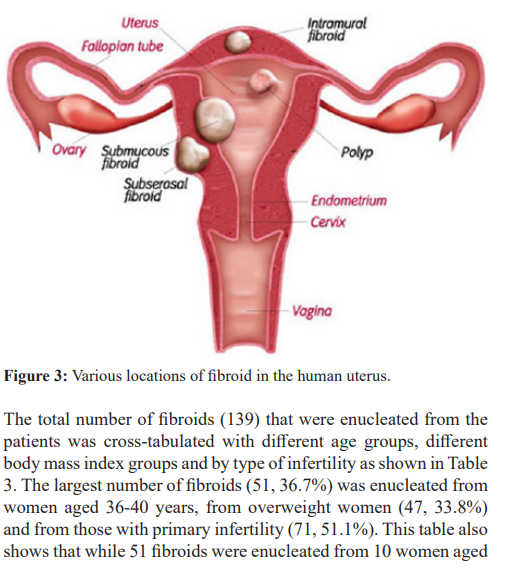
One of the commonest health problems limited to female genital tract, globally and throughout history, is uterine fibroid, a benign gynecological tumor with a prevalence of 25-30% [1]. Fibroid or myoma, as it is referred to medically, are hormone-dependent, resulting from single myoma cells and not from a metastatic process. They may be sub-mucous, sub-serous, intramural or pedunculated. Fibroids may cause symptoms such as menorrhagia, metrorrhagia, pain, hemorrhage and repeated abortions among other symptoms and have been implicated in certain cases of infertility. Up to 30% of women with uterine fibroid are symptomatic [2] with bulk symptoms such as pressure, fullness, urinary symptoms and increased abdominal girth [3]. Based on the observations of Lee et al. [4] and that of Pritts and his co-workers [5], symptoms of fibroid can reduce quality of life in addition to impacting fertility and pregnancy. It has also been observed that location, size and number may influence fibroid-related signs and symptoms [6,7].
In order to achieve a successful conservative treatment of fibroids, functional integrity of the uterus is as important as tumor removal or symptoms relief [8]. Uterine factor, among which is fibroid, plays about a 15-20% role in contributing to female infertility [9]. As stated earlier infertility is one of the outcomes of fibroid. Infertility may be primary if the woman has never conceived before or secondary if she had conceived before. Laparoscopic myomectomy to remove the fibroid and correct infertility in women of child-bearing age, who still wish to get pregnant, has the advantages of less post-operative pain, shorter recovery time [1], reduced blood loss and lower infection rate compared to abdominal myomectomy. Apart from that, some Nigerian studied [10,11] have documented increased incidence and severity of fibroid with pre-menopausal age, making fibroid a common clinical condition encountered in many women of advanced reproductive age. Furthermore, the contemporary tendency of deferred reproduction and an upsurge in the number of women in the advanced child- bearing age have augmented the demand for management of fibroid for preservation of reproductive potential [10-12]. Marret et al. [13] suggested vaginal or laparoscopic myomectomy (LM) in preference to laparotomy for fibroids considered typical on imaging.
It is possible for a woman to have a single fibroid or multiple fibroids of any of the three common types of fibroid (based on their location) such as (i) subserosal, in which the fibroid grows and bulges toward the outside of the uterus, which typically does not affect menstrual flow but can cause significant pelvic and back pain, as well as generalized pressure; (ii) Intramural – in which the fibroid is mostly embedded within the center of the wall of the uterus, the most notorious, and the most prevalent cause of heavier than usual menstrual bleeding, pelvic pain, back pain or generalized pressure: and (iii) Submucous – which grows and bulges toward the inside of the uterus, which is the least common but most problematic of all fibroids, which even in very small growths, can cause heavy bleeding and prolonged menstrual periods and which cannot be detected by clinical investigations alone, hence the need for laparoscopy. However, despite the advantages of LM, abdominal myomectomy is a common modality of treatment for large and symptomatic uterine fibroid in women who wish to retain their fertility, a procedure that is usually associated with complications [14-16].
Furthermore, there is scarcity of data on the role played by the types of infertility, age and Body Mass Index (BMI) in the location, number and sizes of fibroids removed during myomectomy, especially in an African setting. Ageing is a critical factor in the fertility or reproductive profile of a woman as the decline in female fertility is more pronounced after the age of 35 [17]. Body Mass Index has also been linked with female infertility [18]. The objectives of this study is therefore to evaluate (i) association between type of infertility and number of fibroids (ii) mean size of dominant fibroids among these two groups of infertile women and (iii) relationship between uterine size in weeks and type of infertility.
Materials and Method
Detailed description of the materials and methodology used in this study can be found in our previous paper [19] and is available at http://medical-clinical-reviews.imedpub.com/archive.php.
Briefly, this retrospective study was conducted at the endoscopy arm of Nordica Fertility Centre, Lagos, Nigeria (NFC), a private health facility specifically attending to male and female infertility and Assisted Reproduction Technology (ART) which includes in- vitro fertilization (IVF).
All women presenting for IVF are routinely given abdominal, pelvic and uterine ultrasonography assessment prior to treatment for infertility. Between January 2010 and December 2014, 31 women presented with symptoms suggestive of large fibroids. These patients were first counselled and prepared by the Apex Nurse before meeting any of the consultant gynecologists and experts in Assisted Reproduction Technology (ART) employed at NFC. Patients were mostly self-referred to NFC when they hear from others who had successful laparoscopic myomectomy (LM) at this health facility. This was because LM was a relatively new procedure in the country and in most parts of the continent. However, some referrals were from other public or private health facilities within or outside the country. Few of the patients read leaflets on LM from women’s health magazines or saw television advertisements mainly on foreign electronic media.
During their consultation, women were given about 45-min counselling to allay their fears and anxiety on their health conditions and the procedure to remove the fibroid. The patients, either alone or with a spouse, also had a one-on-one talk with any of the specialist gynecologists at NFC. Apart from being specialists, all gynecologists at this health facility are also well-grounded in endoscopy for pelvic imaging and ultrasonography. Some of the comprehensive history taken from the patients included (but were not limited to) demography, occupation, marital status, years trying to conceive, past and current illnesses and medications used, allergy, presenting symptoms of fibroid such as abdominal extension, feeling of bulkiness, pelvic pain, menorrhagia, dysmenorrhea and dysuria.
History taking was followed by general palpation for anemia and lymphadenopathy followed by abdominal palpation for organomegaly. The size of the bulky uterus was determined by measurement with the umbilicus as the reference point. The size was recorded in weeks, mimicking the gravid uterine size. The gynecologist also performed routine auscultation of the chest to detect any respiratory and/or cardiac pathology followed by an examination per vaginam and a proper pelvic assessment. Laparoscopic myomectomy provided ample opportunity to determine the exact location, the diameter (in cm) and quantity of the fibroids. In addition, the LM also helped in determining other fibroid characteristics such as classical, hyper-cellular or degenerated. A combination of the information from given history, physical examination, auscultation, vaginal and pelvic examination and laboratory results helped to determine the management of each patient. Desire for future fertility was considered with the patients before LM was recommended.
All the 31 consecutive infertile women met the inclusion criteria and all necessary procedures were performed under short general anaesthesia using a rigid 20-degree 5-mm hysteroscope with an operative channel for the use of grasping forceps, scissors, or bipolar electrode. Instruments were placed through the operative channel when needed for treatment of pathology after the diagnostic portion had been completed. All patients who satisfied the following criteria were included in the study: (i) confirmation of fibroid by ultrasound scan and (ii) willing and consenting to undergo LM at NFC. Exclusion criteria were: (i) low to very low Packed Cell Volume (ii) other systemic illnesses. The sampling frame was the list of all patients who had LM conducted on them between.
Training
Three data-recording officers were trained to retrieve data from case notes of all patients who had undergone LM at NFC. The one-day training also included data entry, cleaning, coding and importing from Excel spreadsheet into STATA 13 analytical software. They were assisted and supervised by a seasoned obstetrician/gynecologist in the team (OB).
Approval by Ethics Committee
The study was approved by the State’s Ethics Committee. The gynecologists gave comprehensive description of the process and all women signed an informed consent before undergoing the procedure.
Statistical analysis
Age (years) was categorized into ≤30, 31-35, 36-40, 41-45 and 46- 50 and Body Mass Index (BMI kg/m2) into underweight (<18.5), normal (18.5-24.9), overweight (25.0-29.9), and obese (≥30.0). No patient was underweight so this category was eventually omitted. Analysis was done using STATA 13 and the level of significance was set at P<0.05. Descriptive statistics were presented as numbers and percentages for qualitative data and student’s t-test was used to compare the mean and standard deviations for quantitative data of the two groups. Cross-tabulation was performed and the resulting Pearson’s chi-square was used to assess correlation of different proportions of women with primary and secondary infertility. Odds ratio and 95% confidence interval were automatically generated. Multivariate analysis was performed for association between selected dependent variables against other independent variables. Results are presented in Tables, Bar charts and diagrams.
Results
Thirty-one women (means (±) of age and BMI were 38.0 (5.3) years and 27.4 (4.6) kg/m2), who presented for laparoscopic myomectomy at our center were studied (Table 1). Of these 31, 13 (41.9%) presented with primary infertility and 18 (58.1%) with secondary infertility. There was no statistically significant

Discussion
Uterine fibroids are extremely common findings in women of reproductive age [8] and laparoscopic myomectomy (LM), in the hands of an experienced surgeon, is a safe technique, with an extremely low failure rate and good results in terms of the outcome of pregnancy [20].
Laparoscopic myomectomy is a relatively new invention for non-invasive removal of uterine fibroids. Its advantages over open myomectomy include efficacy, low likelihood of uterine rupture, reduced blood loss, lesser post-operative pain and overall complications [21,22]. The adoption of this new approach for the management of uterine fibroids lags behind in the developing world mainly because of cost and probably because of the unfamiliarity and discomfort associated with non-surgical options of myomectomy [23].
In all the subjects of this study, infertility associated with fibroids, was the major reason for LM prior to in-vitro fertilization in consonance with what has been reported [15,24]. There are some major findings in this study. One is that women presenting with fibroids were in their late 30s, were overweight and have been trying to conceive for about six years. The mean age of patients in our study corresponds with what Ezeama et al. [25] reported, though they presented a higher proportion of nulliparous women compared to our study. Although Ekine et al. [26] also shared the same opinion, their patients included more single women than ours. Women presenting with fibroid for LM were also overweight, a finding that is comparable with what Ying et al. [27] described that body mass index, among other variables was positively associated with uterine fibroid. It should be noted, however, that studies in mainly Caucasians have shown diverse outcomes with respect to the association between body mass index and uterine fibroids [28- 32]. Moore et al. [33] however stated a higher proportion of blacks consulting for myomectomy and that mean BMI and uterine weight were higher in them than among Caucasians.
A study suggested that uterine fibroids are probably a hormone- related disease [34] while another study associated obesity to an increase in circulating estrogen and its production [35]. Thus there is protracted time interval when circulating estrogen is devoid of the compensatory effects of progesterone [36]. Infertility was the primary complaint of those who presented for LM in our study. The mean duration of infertility was significantly longer in women with secondary infertility than among those with primary infertility. Obed et al. [15] reported a lower mean duration of infertility of 3.2 ± 2.2 years among women of slightly older age group. Marshall et al. [37] observed that the incidence of uterine fibroids increases widely with age, and infertility, when really caused by uterine fibroids, should occur later in a woman's reproductive life. This observation agrees with findings in our study and may be the potential reason for the high occurrence of infertility among women with secondary infertility as seen in this study. One of the possible mechanisms by which uterine fibroids reduce or compromise fertility may be physically distorting the shape of the cervix, the external and internal os, as well as the cervical canal and thereby lessen the quantity of sperm cells that can pass into the uterus. It is also possible for the uterine fibroids to alter the contour of the uterus which may inhibit the swimming action of the sperm and restrict the movement of the embryo. Furthermore, uterine fibroids, depending on location, may occlude either or both fallopian tubes.
The next major finding in our study concerned the distribution of sites of fibroids. Sub-serosal fibroid was more common among women with secondary infertility than among those with primary infertility a result that tallies with the findings reported by Mettler et al. [1]. Subserosal fibroids do not significantly affect fertility outcomes, and removal may not confer benefit [20]. Location of the fibroid is a probable source of complication of the condition. Because it bulges towards the outside of the uterus, subserosal fibroids may not directly affect menstrual flow but may possibly result in complications such as significant pelvic and back pain episodes, chronic abdominal pain with intermittent spasms, dysuria, constipation, chronic bladder and bowel spasms and even to peritonitis.
In our study, submucosal fibroid was slightly more prominent in secondary than in primary infertility. Klatsky et al. [38] concluded that submucosal fibroid correlates well with reduced pregnancy rate and Pritts et al. [5] stated that fertility outcomes are decreased in women with submucosal fibroids and removal seems to confer benefit in terms of pregnancy rates. However, majority of women in our study presented with intramural fibroid which tallies with the report given by Tan et al. [3]. Two of the established characteristics of fibroids are (i) to influence the contractility of the myometrium and induce a chronic inflammatory reaction thus hindering embryonic implantation [39-43] and can also increase the likelihood of infertility and pregnancy loss and (ii) to possibly alter steroid receptors to affect implantation failure [44]. Intramural fibroids, the most common, may result in heavier menstrual bleeding and pains, especially in the pelvis and back region. One of the consequences of intramural fibroids is menorrhagia, though this is not usually present. In addition, increase in myometrial peristalsis in the presence of intramural fibroid has been reported [41-43]. It is quite interesting that, in our study, the mean sizes of all types of fibroid were bigger among women with primary than those with secondary infertility. Many studies have reported the association between fibroids and infertility [1,16,45-48], but extremely few have ever reported association with different types of infertility. This paper may be the first of such observation being reported in Africa.
Among the 15 women who continued with IVF, one was about to start treatment when this study started. Of the remaining 14, 3 (21.4%) had a positive pregnancy outcome 2 (66.7%) with secondary infertility and 1 (33.3%) with primary infertility. This could possibly be an interplay of various hormones that support pregnancy. It may also be as a result of age, body mass index, duration of infertility or other factors. More research is needed in this area.
Study Limitations
Our study has some limitations that need to be explained. First, the data was secondary in that it was extracted from the medical records of patients. The inherent drawbacks include having to rely on the records as being correct with minimal error. The medical records were in hard copy and not electronic so transcription of writings of the surgeons may have introduced some minimal error. We attempted to correct this as much as possible by having a gynecologist (OB) cross-check all data. Secondly, working from one fertility center limited our sample size to a small quantity of 31 which may have impacted on some statistical analysis. Probably a sub-regional study involving many centers in each country can present a clearer picture of the subject of study. Thirdly, the socio- demographic characteristics of the patients could have been a confounder because more economically buoyant patients consult at this private fertility center.
Conclusion
Our findings suggest that women with primary infertility present with larger quantity, bigger sizes and thus bulkier uterus than women with secondary infertility. Furthermore, data from our study propose that intramural and pedunculated fibroids are more common in primary than in secondary infertility.
References
- Mettler L, Schollmeyer T, Tinelli Complications of Uterine Fibroids and Their Management, Surgical Management of Fibroids, Laparoscopy and Hysteroscopy versus Hysterectomy, Haemorrhage, Adhesions, and Complications. Obstet Gynecol Int. 2012; 2012: 791248.
- Buttram VC Jr, Reiter RC. Uterine leiomyomata: etiology, symptomatology, and management. Fertil Steril. 1981; 36: 433-445.
- Tan N, McClure TD, Tarnay C, et al. Women seeking second opinion for symptomatic uterine fibroid: role of comprehensive fibroid Journal of Therapeutic Ultrasound. 2014; 2: 3.
- Lee DW, Gibson TB, Carls GS, et al. Uterine fibroid treatment patterns in a population of insured Fertil Steril. 2009; 91: 566-574.
- Pritts EA, Parker WH, Olive DL. Fibroids and infertility: an updated systematic review of the Fertil Steril. 2009; 91: 1215-1223.
- Herbst ALMD, Stencheuer MA, Droegemuller Comprehensive Gynecology St Louis: Mosby; 1992.
- Novak Myoma and Other Benign Tumors of the Uterus. Philadelphia Saunders; 1979.
- Gambadauro P, Gudmundsson J, Torrejón R. Intrauterine Adhesions following Conservative Treatment of Uterine Obstetrics and Gynecology International. 2012: 6.
- Palshetkar N, Pai H, Pisat S. Role of hysteroscopy prior to assisted reproductive J Gynecol Endosc Surg. 2009; 1: 27-30.
- Okezie O, Ezegwui HU. Management of uterine fibroids in Enugu, J Obstet Gynaecol. 2006; 26: 363-365.
- Aboyeji AP, Ijaiya MA. Uterine fibroids: A ten-year clinical review in Ilorin, Niger J Med. 2002; 11: 16-19.
- García CR. Management of the symptomatic fibroid in women older than 40 years of age. Hysterectomy or myomectomy? Obstet Gynecol Clin North 1993; 20: 337-348.
- Marret H, Fritel X, Ouldamer L, et Therapeutic management of uterine fibroid tumors: updated French guidelines. Eur J Obstet Gynecol Reprod Biol. 2012; 165: 156-164.
- Geidam AD, Lawan ZM, Chama C, et al. Indications and outcome of abdominal myomectomy in University of Maiduguri Teaching Hospital: Review of ten Niger Med J. 2011; 52: 193-197.
- Obed JY, Bako B, Kadas S, et The benefit of myomectomy in women aged 40 years and above: Experience in an urban teaching hospital in Nigeria. Niger Med J. 2011; 52: 158-162.
- Gávai M, Hupuczi P, Papp [Abdominal myomectomy as an alternative to hysterectomy: analysis of 504 cases]. Orv Hetil. 2006; 147: 971-978.
- The Practice Committee of the American Society for Reproductive Aging and Infertility in women. Fertility and Sterility. 2006; 86: S248.
- Kulie T, Slattengren A, Redmer J, et al. Obesity and women's health: an evidence-based review. J Am Board Fam Med. 2011; 24: 75-85.
- Ajayi A, Ajayi V, Biobaku O, et Laparoscopic Myomectomy: A 6-Year Experience at Nordica Fertility Center, Lagos, Nigeria. J Minim Invasive Gynecol. 2015; 22: S235.
- Jin C, Hu Y, Chen XC, et Laparoscopic versus open myomectomy--a meta-analysis of randomized controlled trials. Eur J Obstet Gynecol Reprod Biol. 2009; 145: 14-21.
- Desai P, Patel Fibroids, infertility and laparoscopic myomectomy. J Gynecol Endosc Surg. 2011; 2: 36-42.
- Lefebvre G, Vilos G, Allaire C, et Clinical Practice Gynaecology Committee, Society for Obstetricians and Gynaecologists of Canada. The management of uterine leiomyomas. Obstet Gynaecol Can. 2003; 25: 396-418.
- Pron New uterine-preserving therapies raise questions about interdisciplinary management and the role of surgery for symptomatic fibroids. Fertil Steril. 2006; 85: 44-55.
- Trivedi P, Abreo M. Predisposing factors for fibroids and outcome of laparoscopic myomectomy in J Gynecol Endosc Surg. 2009; 1: 47-56.
- Ezeama C, Ikechebelu J, Obiechina Nj, et Clinical Presentation of Uterine Fibroids in Nnewi, Nigeria: A 5-year Review. Ann Med Health Sci Res. 2012; 2: 114-118.
- Ekine AA, Lawani LO, Iyoke CA, et Review of the Clinical Presentation of Uterine Fibroid and the Effect of Therapeutic Intervention on Fertility. Review of the Clinical Presentation of Uterine Fibroid and the Effect of Therapeutic Intervention on Fertility. American Journal of Clinical Medicine Research. 2015; 3: 9-13.
- Yang Y, He Y, Zeng Q, et al. Association of body size and body fat distribution with uterine fibroids among Chinese J Womens Health (Larchmt). 2014; 23: 619-626.
- Lumbiganon P, Rugpao S, Phandhu-Fung S, et al. Protective effect of depot-medroxy-progesterone acetate on surgically treated uterine leiomyomas: a multicentre case–control Br J Obstet Gynaecol. 1996; 103: 909-914.
- Parazzini F, Negri E, La Vecchia C, et Reproductive factors and risk of uterine fibroids. Epidemiology. 1996; 7: 440-442.
- Marshall LM, Spiegelman D, Manson JE, et Risk of uterine leiomyomata among premenopausal women in relation to body size and cigarette smoking. Epidemiology. 1998; 9: 511- 517.
- Faerstein E, Szklo M, Rosenshein N. Risk factors for uterine leiomyoma: a practice-based case-control study. I. African- American heritage, reproductive history, body size, and Am J Epidemiol. 2001; 153: 1-10.
- Ross RK, Pike MC, Vessey MP, et Risk factors for uterine fibroids: reduced risk associated with oral contraceptives. Br Med J (Clin Res Ed). 1986; 293: 359-362.
- Moore AB, Flake GP, Swartz CD, et Association of race, age and body mass index with gross pathology of uterine fibroids. J Reprod Med. 2008; 53: 90-96.
- Khan AT, Shehmar M, Gupta JK. Uterine fibroids: current Int J Womens Health. 2014; 6: 95-114.
- Sarwer DB, Spitzer JC, Wadden TA, et Sexual functioning and sex hormones in persons with extreme obesity and seeking surgical and nonsurgical weight loss. Surg Obes Relat Dis. 2013; 9: 997-1007.
- Van den Bosch T, Coosemans A, Morina M, et al. Screening for uterine tumours. Best Pract Res Clin Obstet Gynaecol. 2012; 26: 257-266.
- Marshall LM, Spiegelman D, Barbieri RL, et al. Variation in the incidence of uterine leiomyoma among premenopausal women by age and Obstet Gynecol. 1997; 90: 967-973.
- Klatsky PC, Tran ND, Caughey AB, et Fibroids and reproductive outcomes: a systematic literature review from conception to delivery. Am J Obstet Gynecol. 2008; 198: 357- 366.
- Richards PA, Richards PD, Tiltman AJ. The ultrastructure of fibromyomatous myometrium and its relationship to Hum Reprod Update. 1998; 4: 520-525.
- Rackow BW, Taylor HS. Submucosal uterine leiomyomas have a global effect on molecular determinants of endometrial Fertil Steril. 2010; 93: 2027–2034.
- Kido A, Ascher SM, Hahn W, et T MRI uterine peristalsis: comparison of symptomatic fibroid patients versus controls. Clin Radiol. 2014; 69: 468-472.
- Yoshino O, Nishii O, Osuga Y, et Myomectomy decreases abnormal uterine peristalsis and increases pregnancy rate. J Minim Invasive Gynecol. 2012; 19: 63-67.
- Yoshino O, Hayashi T, Osuga Y, et al. Decreased pregnancy rate is linked to abnormal uterine peristalsis caused by intramural Hum Reprod. 2010; 25: 2475-2479.
- Tocci A, Greco E, Ubaldi Adenomyosis and 'endometrial- subendometrial myometrium unit disruption disease' are two different entities. Reprod Biomed Online. 2008; 17: 281-291.
- Agdi M, Tulandi Endoscopic management of uterine fibroids. Best Pract Res Clin Obstet Gynaecol. 2008; 22: 707- 716.
- amigsurgery.com/gyn-conditions/abno
- sirweb.org/uterine-fibroids/
- fibroidoptions.com/background.html